


The article titled "10 Heart Failure Medications to Improve Your Health" gently explores the various medications available to manage heart failure and enhance patient health outcomes. It highlights the importance of personalized treatment approaches, emphasizing how tailored medication management can significantly improve heart failure symptoms. This not only helps to reduce hospitalizations but also enhances the quality of life for patients, especially our elderly loved ones.
Have you or someone you care about been feeling overwhelmed by heart failure? You're not alone. Understanding the right medications can be a vital step towards feeling better. By focusing on personalized care, we can address individual needs and concerns, ensuring that each patient receives the support they deserve.
In addition to this, the article reassures readers that with the right medication management, there is hope for a brighter, healthier future. It encourages patients to reach out for support, knowing that compassionate care is available to guide them through their journey. Remember, taking the first step towards managing heart failure is an important one, and you don’t have to do it alone.
Heart failure is a complex and often daunting condition that affects millions, particularly the elderly, who face unique challenges in managing their health. As research continues to evolve, the landscape of heart failure medications is expanding, offering new hope for improved outcomes and quality of life. This article delves into ten essential heart failure medications that not only enhance treatment efficacy but also emphasize the importance of personalized care strategies.
With so many options available, how can patients and caregivers navigate this intricate web of therapies to find the most effective solutions for their specific needs? We understand that this journey can feel overwhelming, but you are not alone in seeking the best care.
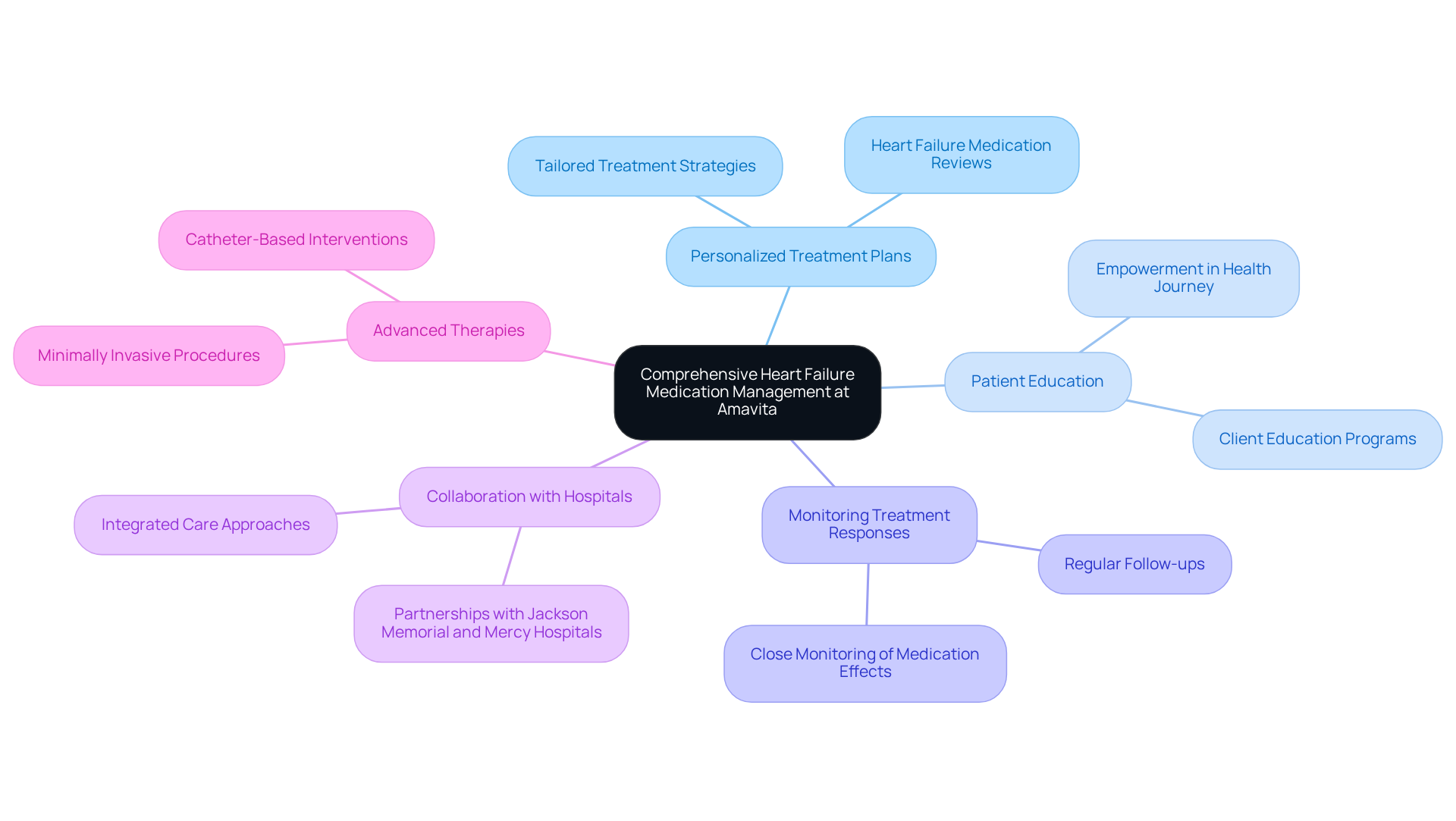
At Amavita Heart and Vascular Health, we are wholeheartedly dedicated to providing comprehensive treatment management for individuals facing cardiac issues, particularly our elderly patients, who often encounter unique challenges in their care. By emphasizing advanced therapies and personalized care, we seamlessly integrate state-of-the-art treatments with compassionate support. Our skilled team is committed to ensuring that each patient receives tailored treatment plans that specifically address their health needs, ultimately enhancing adherence and improving outcomes.
Our effective programs for managing cardiac dysfunction highlight the importance of personalized treatment approaches. Research indicates that individualized treatment plans utilizing heart failure medication can significantly improve heart failure outcomes, reducing hospital visits and enhancing quality of life. As we look toward optimal approaches for 2025, we emphasize regular reviews of heart failure medication, client education, and close monitoring of treatment responses—essential elements for improving therapy in older adults.
Amavita proudly offers advanced outpatient procedures, including minimally invasive valve repairs and catheter-based interventions, allowing individuals to return home the same day. Our cardiologists advocate for a client-focused strategy, underscoring that individualized care is crucial for elderly individuals dealing with heart failure medication. As one expert wisely noted, "Customizing treatment to the individual not only enhances adherence but also empowers individuals in their health journey." This philosophy is at the heart of Amavita's approach, ensuring that every patient receives the attention and care they truly deserve in . Additionally, we collaborate with Jackson Memorial and Mercy Hospitals to further enhance the quality of care we provide.
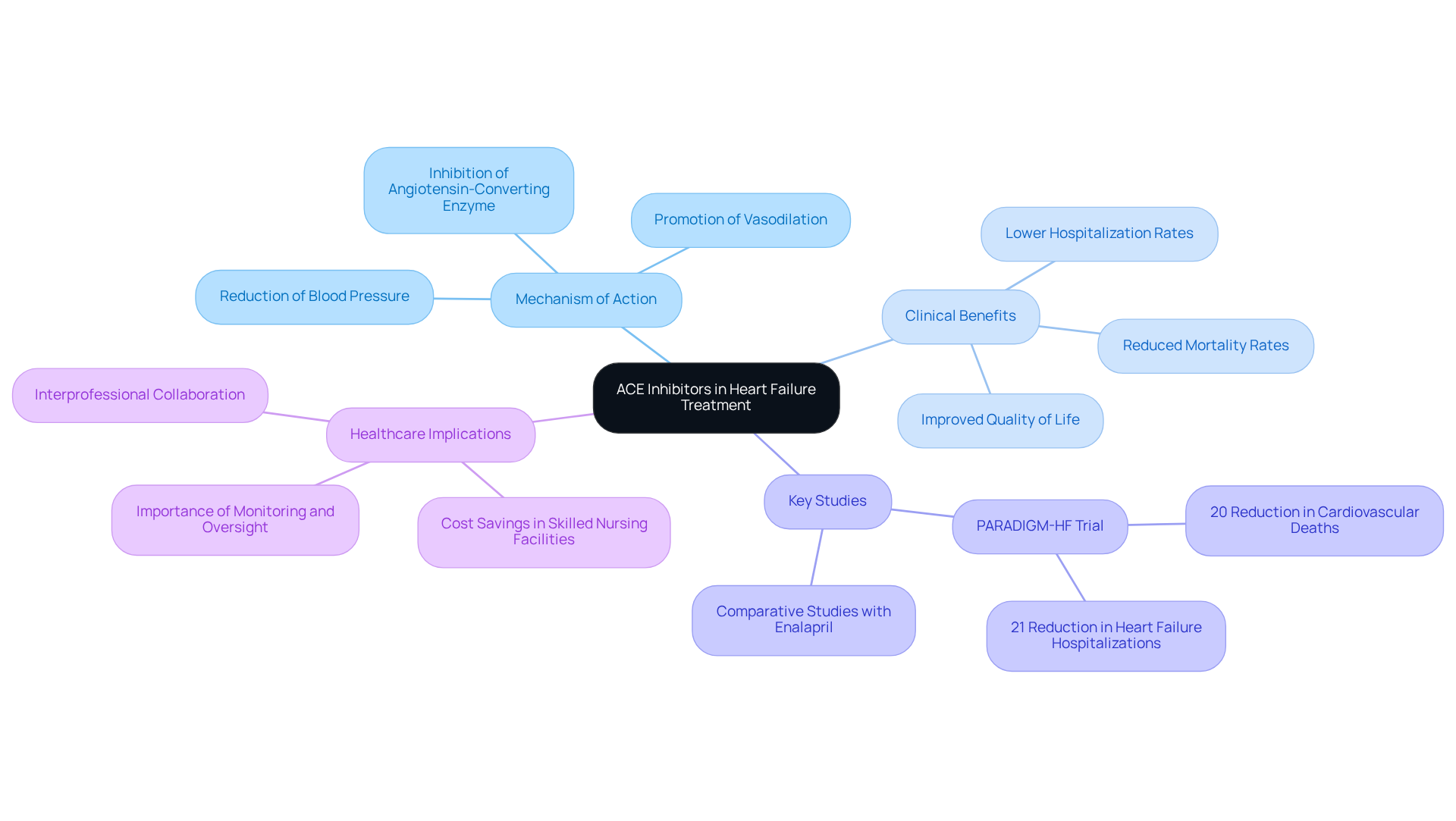
ACE inhibitors, such as lisinopril and ramipril, play a vital role in managing cardiac dysfunction, addressing a concern many may have about their heart health. By inhibiting the angiotensin-converting enzyme, these medications promote vasodilation and lower blood pressure, which in turn reduces the workload on the heart and enhances cardiac output. Clinical studies have shown that these medications significantly lower hospitalization rates and mortality among individuals with cardiac dysfunction, providing hope for better health outcomes.
For instance, the PARADIGM-HF trial revealed that LCZ696, a new treatment option, decreased cardiovascular fatalities by 20% compared to traditional ACE inhibitors like enalapril. This finding is particularly encouraging for older individuals, as ACE inhibitors have demonstrated a significant reduction in cardiovascular hospitalizations within this group. Regular use of heart failure medication is associated with improved management of cardiac symptoms and an overall enhancement in quality of life, making them essential components of treatment for those at risk.
Furthermore, recent research indicates that heart failure medication, including drugs such as lisinopril and ramipril, not only improve survival rates but also help enhance functional capacity in individuals with heart failure. In the context of Amavita's CardioElite™ SNF Program, these treatments are crucial in addressing the cardiovascular challenges faced by skilled nursing facilities, including high readmission rates and care coordination issues. This approach has contributed to a remarkable 93% reduction in readmissions and significant cost savings, ultimately enhancing patient outcomes through advanced diagnostic tools and seamless care coordination.
If you or a loved one are navigating these challenges, know that there are effective treatments available, and support is always within reach. Your matters, and together, we can work towards a brighter, healthier future.
For many individuals facing challenges with ACE inhibitors, angiotensin II receptor blockers (ARBs), such as losartan and valsartan, offer a compassionate alternative. These medications work by inhibiting the effects of angiotensin II, promoting vasodilation, and ultimately helping to lower blood pressure. This is crucial for managing cardiac dysfunction. Recent studies have shown that heart failure medication, such as ARBs, can significantly improve outcomes for those experiencing heart failure, particularly in patients with preserved ejection fraction.
However, it’s important to approach their use with care. A meta-analysis involving over 25,000 individuals indicated that ARB therapy did not significantly reduce total mortality or hospitalizations compared to placebo. This finding underscores the need for thoughtful consideration when choosing treatment options. In practice, ARBs are often recommended for individuals who experience side effects from ACE inhibitors, as they tend to be better tolerated.
Yet, combining ARBs with ACE inhibitors may increase the risk of withdrawals due to adverse effects, without offering benefits in reducing total mortality or hospital admissions. While ARBs like losartan and valsartan have their advantages, ACE inhibitors should still be viewed as the primary treatment due to their in lowering mortality and morbidity in patients with cardiac issues.
Ultimately, the choice between ARBs and ACE inhibitors should be guided by individual responses and tolerability. This personalized approach ensures that each patient receives the most appropriate care for managing their cardiovascular conditions. Remember, you are not alone in this journey; reaching out for support can make a significant difference in your health and well-being.

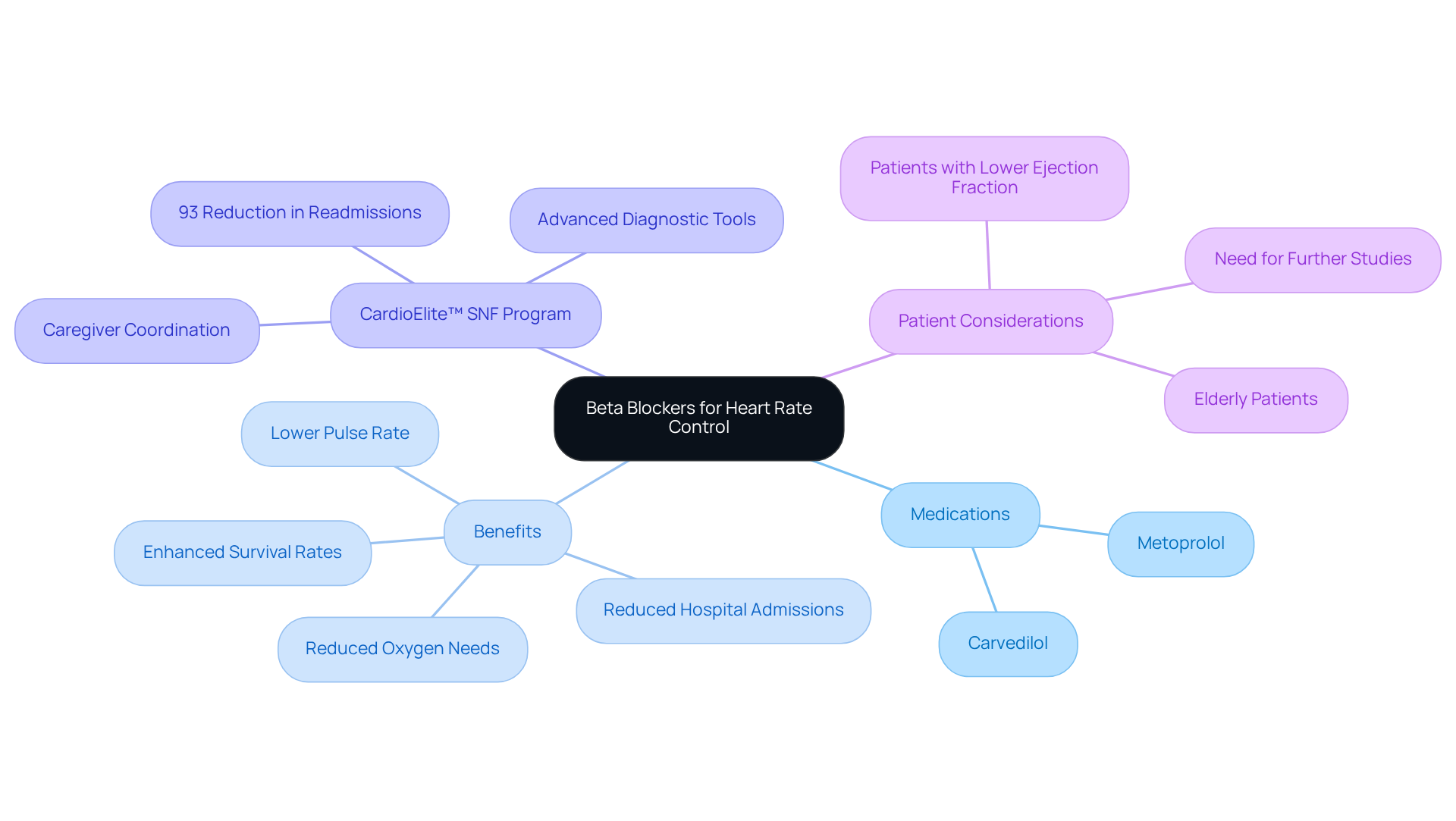
Beta blockers, like carvedilol and metoprolol, play a vital role in managing cardiac dysfunction, especially for our elderly loved ones. They work by gently lowering the pulse rate and reducing the heart's oxygen needs, which is crucial for those facing cardiac insufficiency. Studies have shown that these medications can significantly [enhance survival rates and reduce hospital admissions for individuals with heart failure](https://nature.com/articles/s41598-025-17483-3), particularly those with a lower ejection fraction. This is especially beneficial for older adults, who often experience higher pulse rates and increased cardiac strain.
Through Amavita's CardioElite™ SNF Program, we are dedicated to transforming cardiac care. By implementing advanced diagnostic tools and promoting seamless coordination among caregivers, we have achieved an impressive 93% reduction in readmissions. This program not only addresses the cardiovascular challenges faced by skilled nursing facilities but also enhances the overall health outcomes for our elderly residents. We are committed to ensuring that they receive the comprehensive care they truly deserve.
If you or a loved one is navigating the complexities of heart health, know that support is available. We understand the concerns that come with cardiac issues, and we are here to provide the needed to improve quality of life. Together, we can make a difference in your journey towards better heart health.
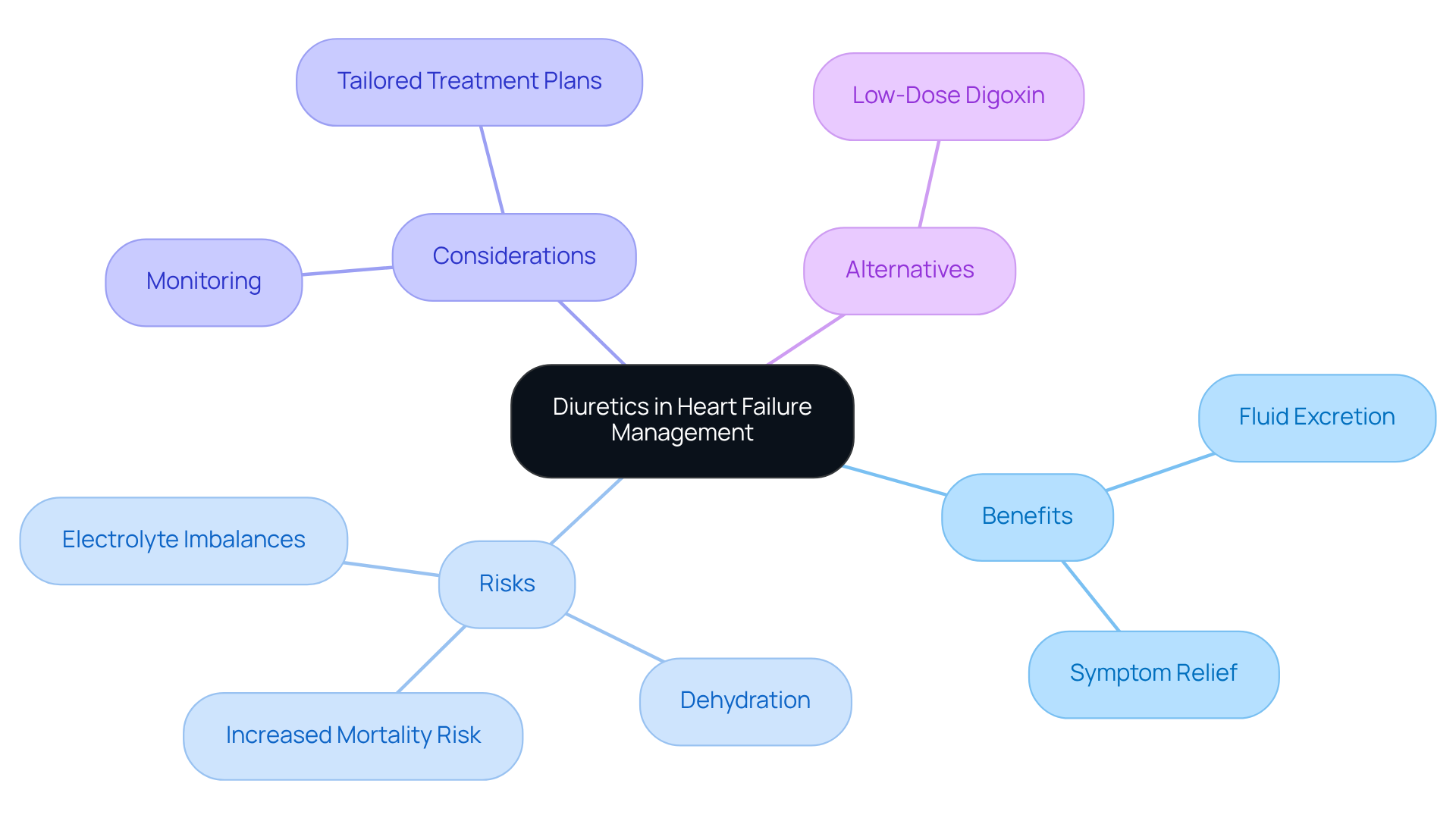
Diuretics, such as furosemide and torsemide, are essential heart failure medications that help individuals manage fluid retention, particularly among our elderly population. These heart failure medications assist in the excretion of excess fluid through the kidneys, providing relief from uncomfortable symptoms such as swelling and shortness of breath. However, it's important to approach their use with care, as older adults may face complications such as electrolyte imbalances and dehydration. Recent clinical evidence highlights the need for tailored treatment plans, as long-term diuretic use has been associated with a concerning 31% increased risk of death and higher hospitalization rates in this group.
Healthcare professionals emphasize that while diuretics, a type of heart failure medication, are vital for alleviating symptoms, it’s worth reconsidering their regular use in individuals who are asymptomatic or only mildly symptomatic. As one expert wisely noted, "Clinicians might also consider adding low-dose digoxin, instead of increasing the dose of diuretics, to relieve HF symptoms." Thus, ongoing monitoring and are crucial in ensuring the best possible outcomes for elderly individuals facing cardiac challenges. Remember, you are not alone in this journey; support is available to help you navigate your health concerns with confidence.
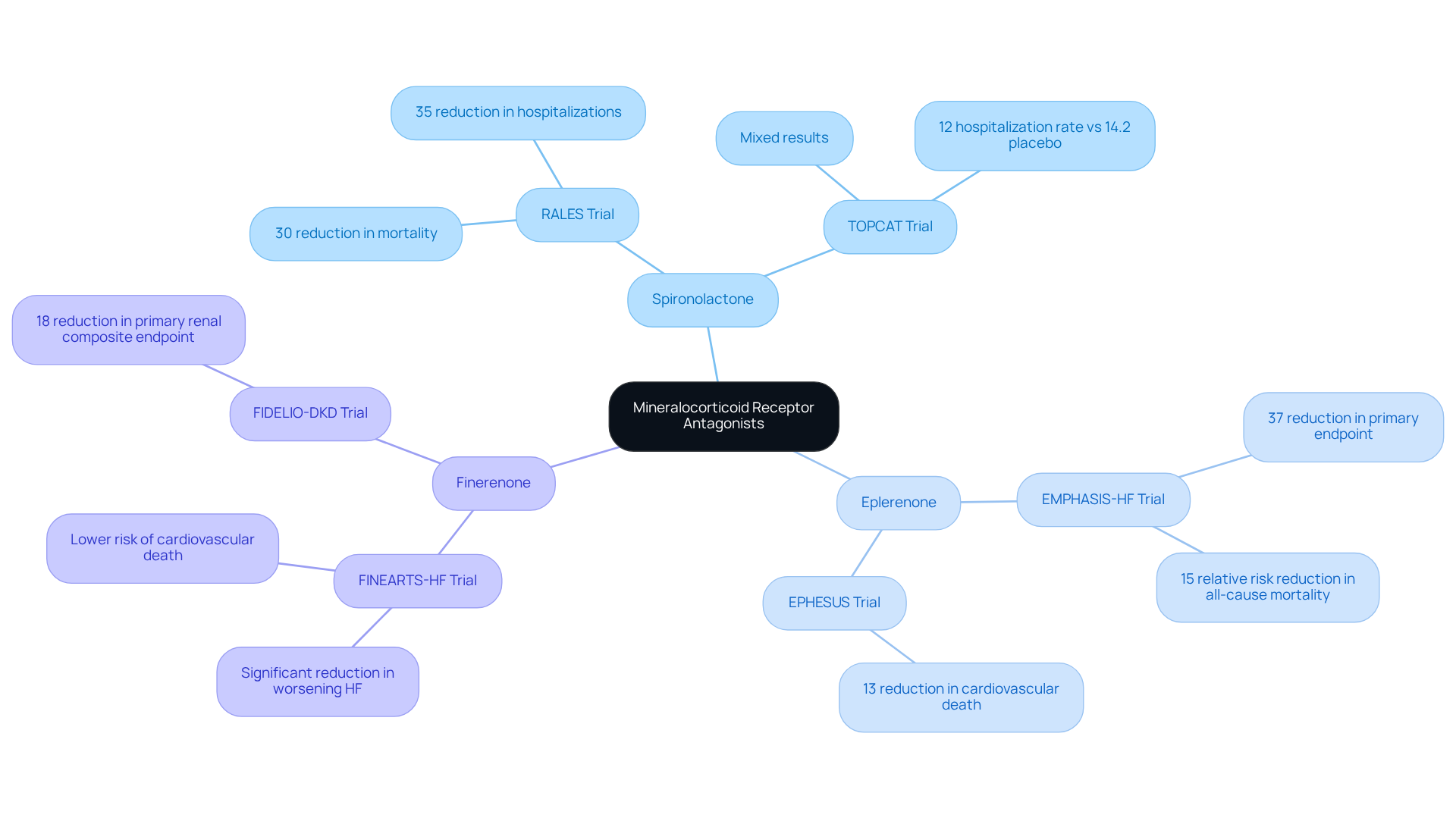
Mineralocorticoid receptor antagonists (MRAs), such as spironolactone and eplerenone, have become recognized as vital components in managing cardiac dysfunction. These medications work by blocking the effects of aldosterone, a hormone that can cause fluid retention and harmful changes in the heart, ultimately improving outcomes for individuals facing these challenges. Recent studies highlight how MRAs can significantly reduce mortality rates among cardiac patients, especially those with reduced ejection fraction (HFrEF). For instance, the RALES trial showed that spironolactone therapy resulted in a 30% relative decrease in mortality and a 35% drop in hospitalizations due to worsening heart conditions. Similarly, the EMPHASIS-HF trial revealed that eplerenone lowered the primary endpoint by 37%, reinforcing its effectiveness in alleviating cardiac symptoms.
In addition to this, the FINEARTS-HF trial examined finerenone, a newer non-steroidal MRA, in patients with heart failure with preserved ejection fraction (HFpEF) and mildly reduced ejection fraction (HFmrEF). This trial demonstrated that finerenone significantly lowered the risk of worsening heart conditions and , highlighting its potential benefits across various cardiac profiles. Overall, MRAs have shown a remarkable ability to reduce hospitalization rates, with a pooled hazard ratio of 0.77 for cardiovascular mortality or cardiac hospitalization. This establishes them as a cornerstone in managing cardiac issues. As our understanding of MRAs continues to evolve, their integration into treatment plans is expected to enhance the quality of care for individuals facing cardiac challenges, offering hope and support for a better future.
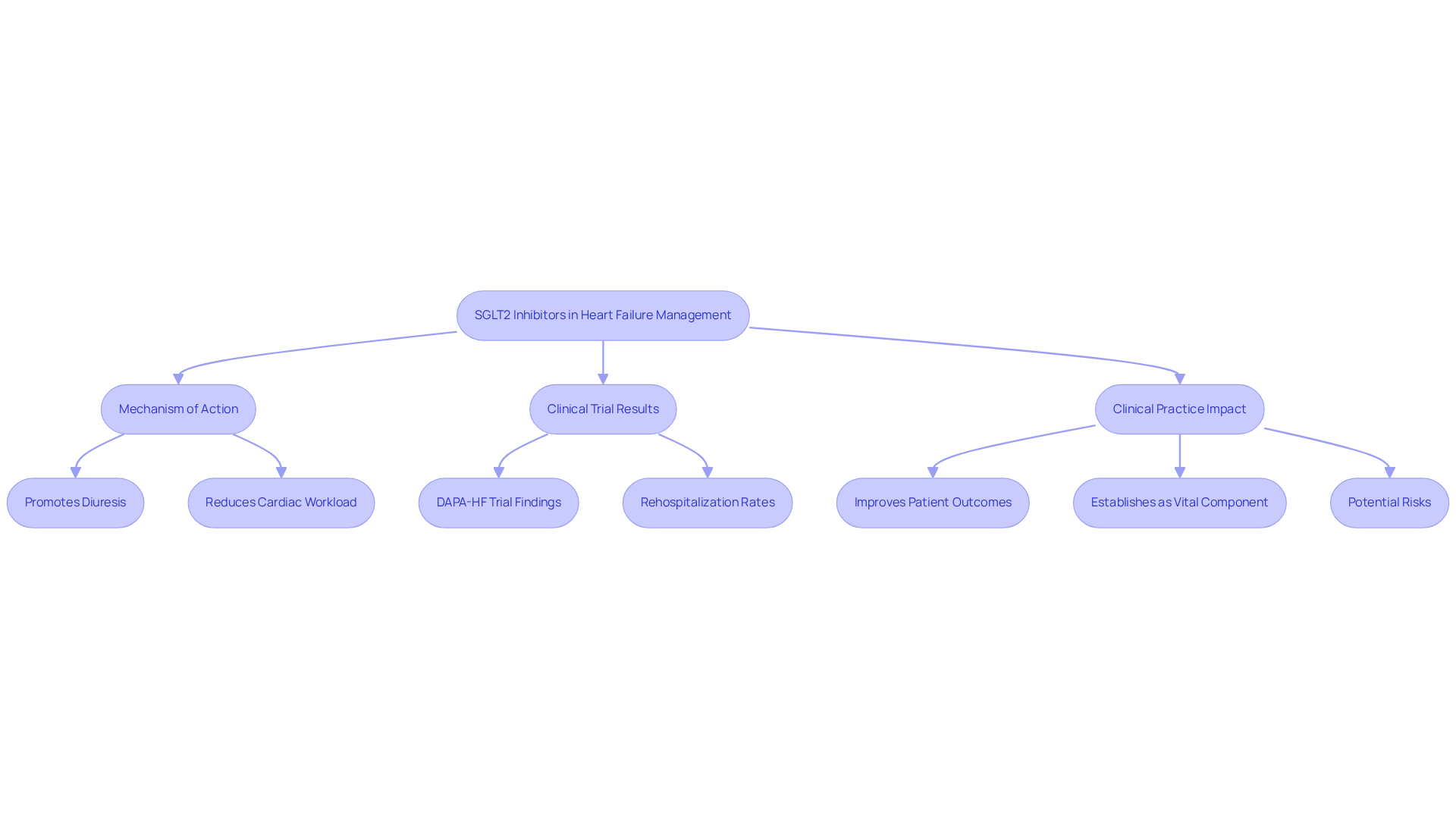
SGLT2 inhibitors, including empagliflozin and dapagliflozin, have emerged as transformative options in managing cardiac dysfunction. Initially developed for diabetes, these medications have shown remarkable cardiovascular benefits, significantly reducing cardiac hospitalizations and improving renal outcomes. Their mechanism of action promotes diuresis, alleviating fluid overload and decreasing cardiac workload, which is crucial for individuals facing cardiac insufficiency.
Recent studies underscore the effectiveness of SGLT2 inhibitors in enhancing patient outcomes. For instance, the DAPA-HF trial revealed that dapagliflozin reduced cardiovascular rehospitalization and mortality in patients with reduced ejection fraction (HFrEF). Specifically, cardiovascular death or worsening heart failure occurred in 10.9% of the dapagliflozin group compared to 12.7% in the placebo group, showcasing a weighted hazard ratio of 0.75. This indicates a 25% lower risk of death among those using SGLT2 inhibitors.
Furthermore, starting SGLT2 inhibitors during hospitalization has been shown to significantly decrease rehospitalization rates. In a recent analysis, cardiovascular rehospitalization was 22.3% for patients treated with SGLT2 inhibitors during their hospital stay, compared to 44.4% for those who began treatment after discharge. This suggests that early intervention with SGLT2 inhibitors can lead to .
Experts highlight the importance of these medications in routine clinical practice. As noted by Prof. Vass Vassiliou, SGLT2 inhibitors not only reduce hospitalizations due to cardiac issues but also improve overall survival rates, establishing them as a vital component of cardiac management strategies. However, it is essential to be aware of potential risks associated with SGLT2 inhibitors, such as symptomatic hypotension and worsening renal function, to provide a balanced perspective on their use. Incorporating these medications into treatment plans represents significant progress in managing cardiovascular conditions, especially for individuals with concurrent diabetes or kidney problems.
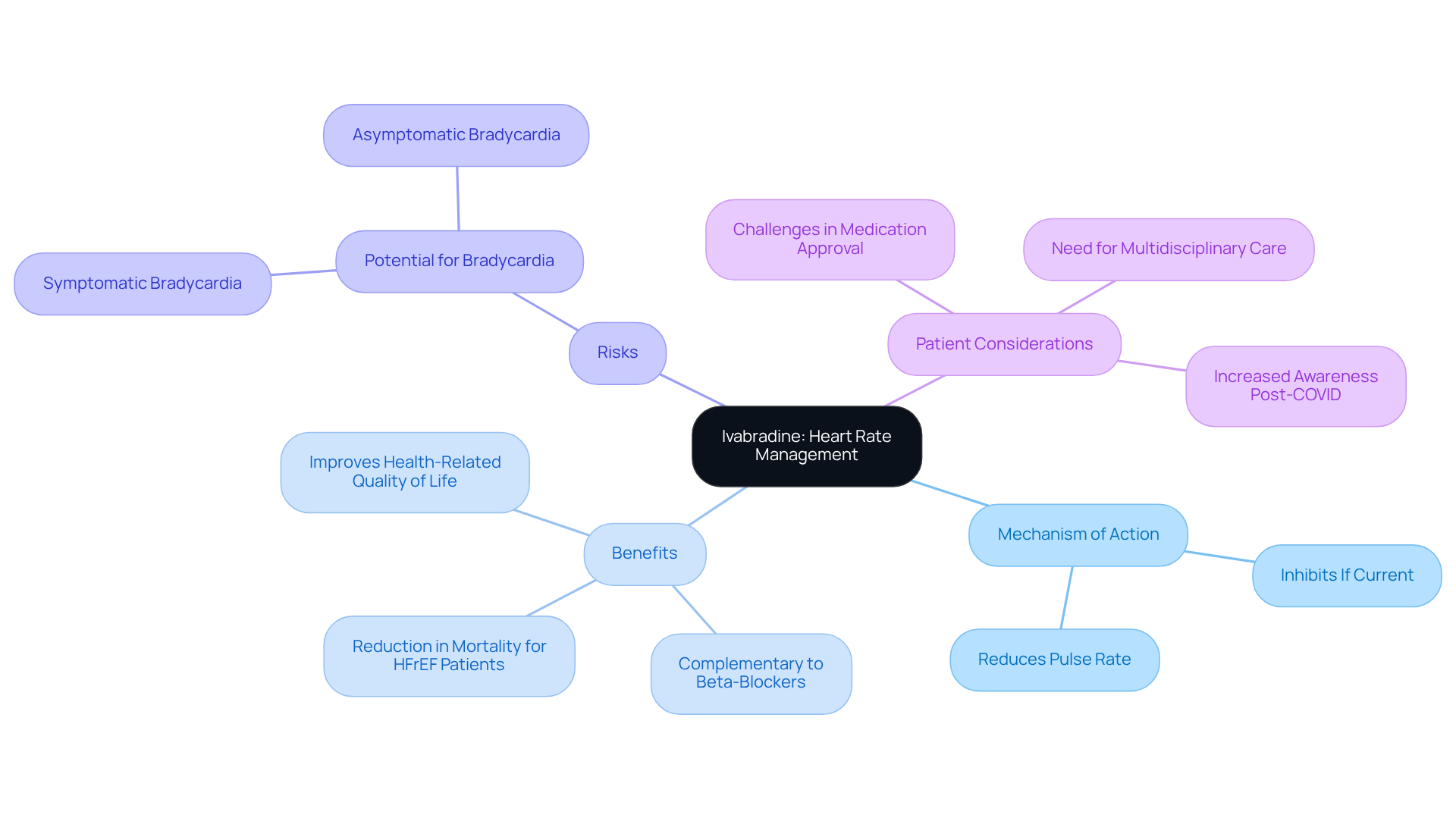
Ivabradine is a unique medication that plays a vital role in managing cardiac dysfunction, particularly for those experiencing elevated pulse rates. By selectively inhibiting the If current in the sinoatrial node, it effectively reduces pulse rate without affecting blood pressure. This makes ivabradine a valuable option for individuals who still experience symptoms despite receiving optimal beta-blocker treatment, providing an additional heart failure medication for effectively managing heart-related issues.
Recent observational studies have shown that ivabradine is associated with a significant reduction in mortality for individuals with reduced ejection fraction (HFrEF). Given that approximately 64 million people around the world are affected by cardiac dysfunction, the importance of effective treatments like ivabradine cannot be overstated. While the benefits of ivabradine are substantial, it is essential to be aware of the , an important consideration for ensuring patient safety.
A systematic literature review has further assessed the efficacy and safety of ivabradine, reinforcing its importance as a key component of heart failure medication, especially for those who find traditional therapies challenging. If you or a loved one are navigating these health concerns, know that support is available. Reaching out for help can make all the difference in managing your heart health effectively.
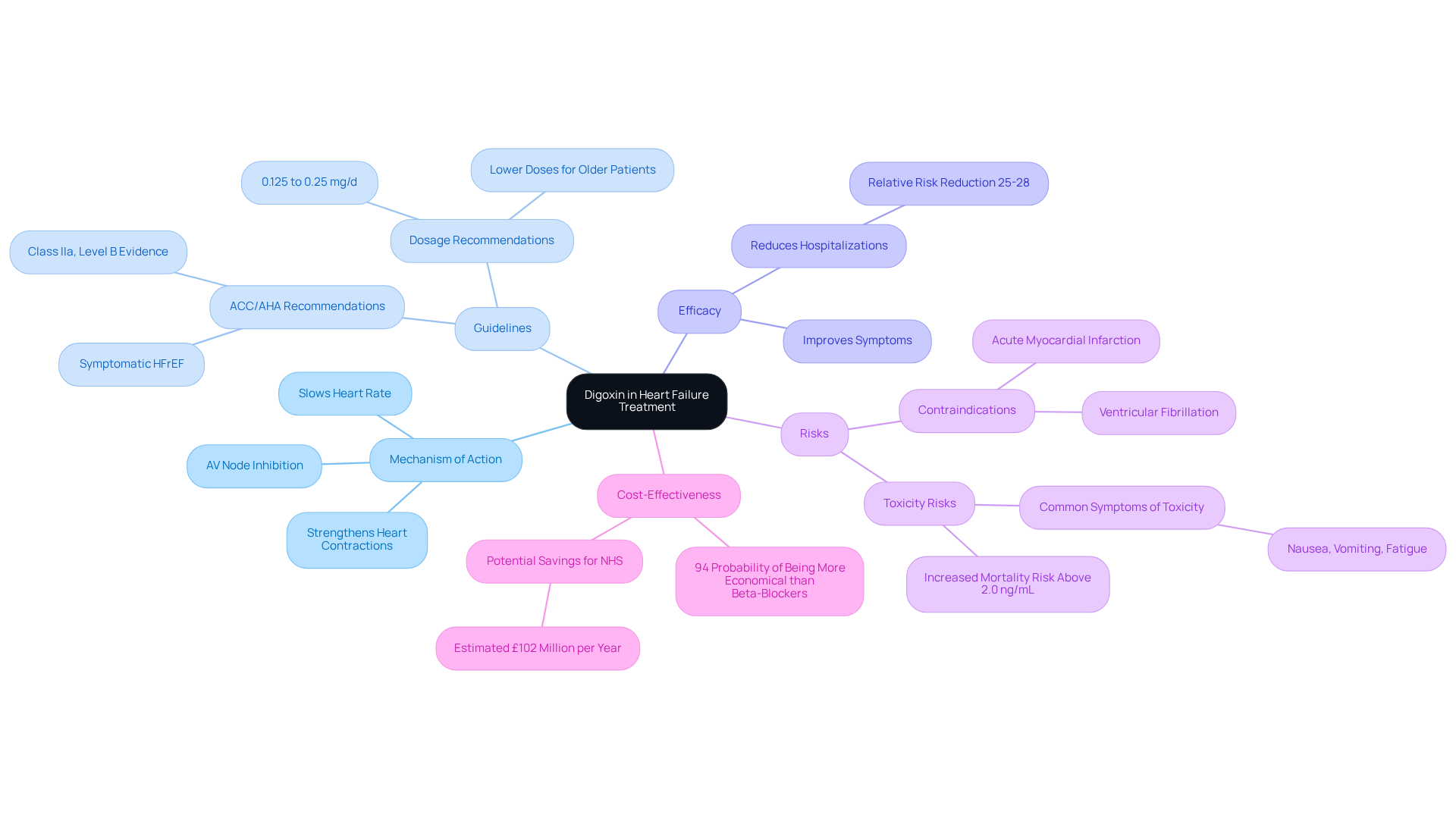
Digoxin, a time-honored medication in managing cardiac dysfunction, continues to be an important part of modern treatment plans. This cardiac glycoside works by increasing the strength of heart contractions and slowing the heart rate, offering significant benefits for those experiencing cardiac insufficiency and atrial fibrillation. While newer therapies have emerged, digoxin remains a for individuals who may not respond well to first-line treatments.
It’s crucial to understand that, although digoxin can be effective, it does not reduce mortality rates. Therefore, it should be used cautiously in individuals without cardiac dysfunction, as it may lead to worse outcomes. The American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend digoxin for those with symptomatic cardiac dysfunction and reduced ejection fraction (HFrEF), particularly for individuals who continue to experience symptoms despite optimal treatment with neurohormonal antagonists (Class IIa, Level of Evidence B).
Recent studies have shown that digoxin can improve symptoms and reduce hospitalizations in individuals with HFrEF, indicating a relative risk reduction of 25-28%. Additionally, its cost-effectiveness is noteworthy, with a 94% probability of being more economical compared to beta-blockers at the standard quality-adjusted life year threshold.
As healthcare professionals, it is essential to navigate the complexities of cardiac dysfunction treatment with care. Understanding digoxin's pharmacology, its potential risks, including toxicity, and its role in managing atrial fibrillation is vital for optimizing outcomes for our patients. We are here to support you and ensure that you receive the best possible care tailored to your needs.
Customized drug management is vital for enhancing cardiovascular treatment, particularly for older individuals who may have unique concerns. By taking into account individual traits such as age, comorbidities, and specific types of heart failure, healthcare providers can create personalized treatment plans that not only improve efficacy but also minimize side effects. This tailored approach has shown significant improvements in clinical outcomes. For instance, individuals utilizing remote digital programs have experienced remarkable advancements in their treatment management without an increase in hospital admissions or emergency visits.
Furthermore, research indicates that nearly half of U.S. counties lack a cardiologist, underscoring the need for scalable solutions that can reach individuals in underserved areas. Healthcare professionals emphasize that timely adjustments to treatments can lead to longer lives and fewer hospitalizations, reinforcing the commitment to compassionate, patient-centered care exemplified by Amavita. By prioritizing tailored heart failure medication regimens, we can enhance the quality of life for heart failure patients, ensuring they receive the best possible care.
Are you or a loved one feeling uncertain about your cardiovascular health? Remember, you are not alone, and there are dedicated professionals ready to support you. Together, we can and find the best path forward.

Effective management of heart failure relies on integrating personalized medication strategies that meet the unique needs of each patient. By taking a comprehensive approach, healthcare providers can significantly enhance outcomes for individuals facing cardiac challenges, especially within the elderly population. Emphasizing tailored treatment plans, the importance of adherence, and continuous monitoring of responses makes the potential for improved quality of life and reduced hospitalizations a tangible reality.
This article has explored a variety of heart failure medications, such as ACE inhibitors, ARBs, beta blockers, diuretics, MRAs, SGLT2 inhibitors, ivabradine, and digoxin. Each medication plays a crucial role in addressing specific aspects of heart failure, from managing fluid retention to improving heart function and reducing mortality rates. As advancements continue to emerge, the significance of personalized care becomes increasingly evident, particularly in optimizing treatment plans for diverse patient profiles.
Ultimately, the journey toward better heart health involves collaboration between patients and healthcare professionals, fostering an environment of support and education. Individuals are encouraged to seek guidance and explore their treatment options, ensuring they are not alone in navigating their health challenges. As the landscape of heart failure management evolves, embracing personalized medication management will remain essential in achieving improved health outcomes and empowering patients on their road to recovery.
What is the focus of Amavita Heart and Vascular Health?
Amavita Heart and Vascular Health is dedicated to providing comprehensive treatment management for individuals facing cardiac issues, particularly elderly patients, by emphasizing advanced therapies and personalized care.
How does Amavita ensure effective management of heart failure?
Amavita emphasizes personalized treatment approaches, regular reviews of heart failure medication, client education, and close monitoring of treatment responses to improve therapy in older adults.
What outpatient procedures does Amavita offer?
Amavita offers advanced outpatient procedures, including minimally invasive valve repairs and catheter-based interventions, allowing individuals to return home the same day.
What role do ACE inhibitors play in heart failure treatment?
ACE inhibitors, such as lisinopril and ramipril, help manage cardiac dysfunction by promoting vasodilation, lowering blood pressure, reducing the workload on the heart, and enhancing cardiac output.
What are the benefits of using ACE inhibitors?
Clinical studies show that ACE inhibitors significantly lower hospitalization rates and mortality among individuals with cardiac dysfunction, improving management of cardiac symptoms and quality of life.
What is the significance of the PARADIGM-HF trial?
The PARADIGM-HF trial revealed that LCZ696, a new treatment option, decreased cardiovascular fatalities by 20% compared to traditional ACE inhibitors, highlighting the importance of these medications for older individuals.
What are Angiotensin II Receptor Blockers (ARBs), and how do they function?
ARBs, such as losartan and valsartan, are alternatives to ACE inhibitors that work by inhibiting the effects of angiotensin II, promoting vasodilation, and helping to lower blood pressure.
Are ARBs as effective as ACE inhibitors?
While ARBs can improve outcomes for those with heart failure, studies indicate they do not significantly reduce total mortality or hospitalizations compared to placebo, making ACE inhibitors the primary treatment choice.
What should guide the choice between ARBs and ACE inhibitors?
The choice should be guided by individual responses and tolerability, ensuring that each patient receives the most appropriate care for managing their cardiovascular conditions.