


The article titled "10 Essential Tips for Managing Peripheral Vascular Disease" offers compassionate guidance for those navigating this condition. It highlights the significance of making lifestyle changes, such as quitting smoking and incorporating regular physical activity into daily routines. These adjustments are vital for alleviating symptoms and minimizing complications related to peripheral vascular disease. Throughout the article, various statistics and expert recommendations provide reassurance and support, fostering a sense of understanding and care for the reader's journey.
Peripheral vascular disease (PVD) poses a silent yet significant health threat, especially for older adults. Often, it remains undetected until serious complications emerge, leaving many feeling anxious about their health. As blood vessels narrow and restrict blood flow, individuals may experience discomfort, pain, and an increased risk of severe outcomes, such as limb loss. This article aims to unveil essential strategies for managing PVD effectively. We will explore:
How can individuals take proactive steps to safeguard their vascular health and enhance their quality of life amidst these challenges? By addressing these concerns, we can empower you to take control of your health and well-being. Together, let’s navigate the path to better vascular health with compassion and understanding.
At Amavita Heart and Vascular Health, we are deeply committed to providing exceptional treatment for individuals facing peripheral vascular disease. Guided by a highly experienced geriatric cardiologist, our practice combines cutting-edge medical techniques with a compassionate, patient-centered approach. This dedication ensures that each individual receives the tailored attention they deserve throughout their treatment journey.
We focus on , such as venous ablation for varicose veins and comprehensive diagnostic testing. These methods not only enhance comfort but also significantly reduce recovery times, making us a favored choice for effective management of peripheral vascular disease. Have you ever wondered how advancements in cardiovascular care can impact your health? Innovative techniques and technologies empower us to achieve successful treatment outcomes, offering you renewed hope.
Geriatric cardiologists emphasize that these minimally invasive options provide significant advantages. They enable individuals to return to their daily activities more quickly while minimizing the risks associated with traditional surgical procedures. Furthermore, our commitment to community outreach and innovative research ensures that you receive not only the highest quality clinical care but also the support you need to improve your quality of life. Together, we can navigate your health journey with understanding and care.
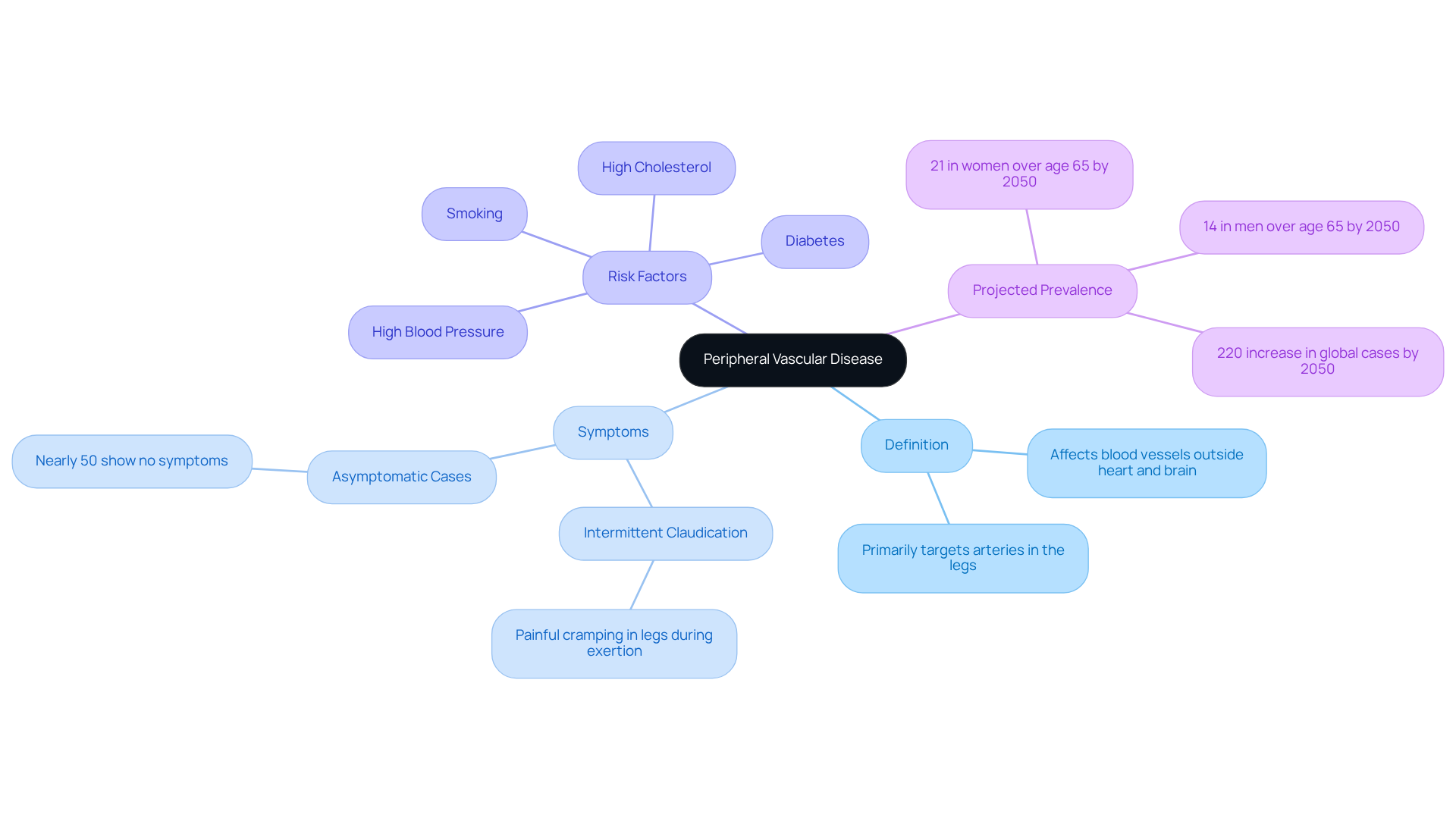
Peripheral vascular disease is a condition that affects the blood vessels outside the heart and brain, primarily targeting the arteries in the legs. This narrowing of blood vessels, a characteristic of peripheral vascular disease, significantly restricts blood flow, which can lead to discomfort and pain, especially during activities like walking. For seniors, the consequences of peripheral vascular disease can be serious, increasing the risk of complications such as limb amputation and cardiovascular events.
Understanding peripheral vascular disease is essential for early detection and effective management. Did you know that nearly 50% of individuals diagnosed with peripheral vascular disease may not show any symptoms? This highlights the importance of awareness. Furthermore, patients suffering from peripheral vascular disease face a threefold greater risk of stroke, underscoring the need for proactive health measures.
Vascular specialists stress the importance of recognizing the signs of peripheral vascular disease, such as , which presents as painful cramping in the legs during exertion. Dr. David G. Armstrong, a respected expert in this field, notes that addressing metabolic health and lifestyle factors can significantly reduce the risks associated with PVD.
The underlying causes of peripheral vascular disease are often related to atherosclerosis, where fatty deposits build up in the arteries, leading to decreased blood flow. Major risk factors include:
As we look ahead, the prevalence of peripheral vascular disease among older adults is projected to exceed 21% in women and 14% in men over age 65 by 2050. This makes targeted interventions and lifestyle changes critical.
In summary, understanding the causes and effects of peripheral vascular disease, as well as its impact on blood flow, is vital for elderly patients. By fostering awareness and encouraging early intervention, individuals can take meaningful steps to manage their cardiovascular health and enhance their quality of life. Remember, you are not alone in this journey; support is available to help you navigate your health concerns.
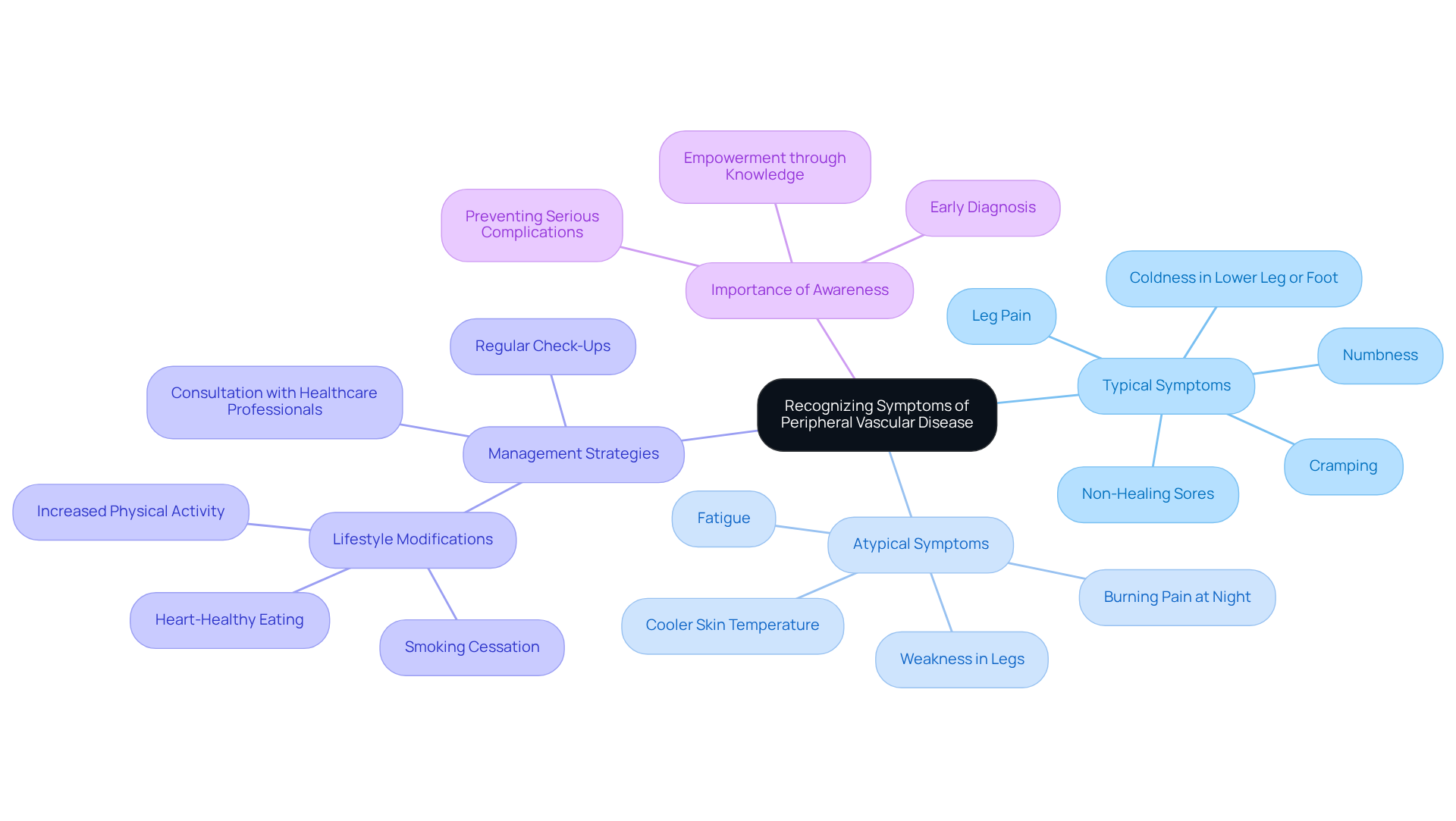
Peripheral vascular condition (PVD) can often present with subtle yet significant symptoms that might easily be overlooked. Have you ever experienced leg pain or cramping during physical activities? Perhaps you’ve noticed numbness or weakness in your legs, or felt coldness in your lower leg or foot? Non-healing sores or wounds can also be a concern. Alarmingly, only about 25% of individuals with PVD experience typical symptoms, while over 50% may have atypical signs that go unnoticed. This highlights the critical need for awareness, particularly among older adults, who are at a .
Recognizing these symptoms early can lead to timely diagnosis and treatment, significantly enhancing your quality of life. For instance, many individuals who mention intermittent claudication—discomfort in the legs during physical activity that alleviates with rest—often find that early intervention can halt the progression of the condition. In fact, lifestyle modifications such as smoking cessation and increased physical activity have proven effective in managing early-stage PVD.
Healthcare professionals emphasize that understanding and recognizing these signs is vital. Routine check-ups and conversations with your primary care physician can assist you in managing peripheral vascular disease, potentially preventing serious complications such as limb loss. By being proactive and attentive to your body, you can take control of your vascular health and enhance your overall well-being. Remember, you are not alone on this journey; support is available, and taking these steps can lead to a healthier future.
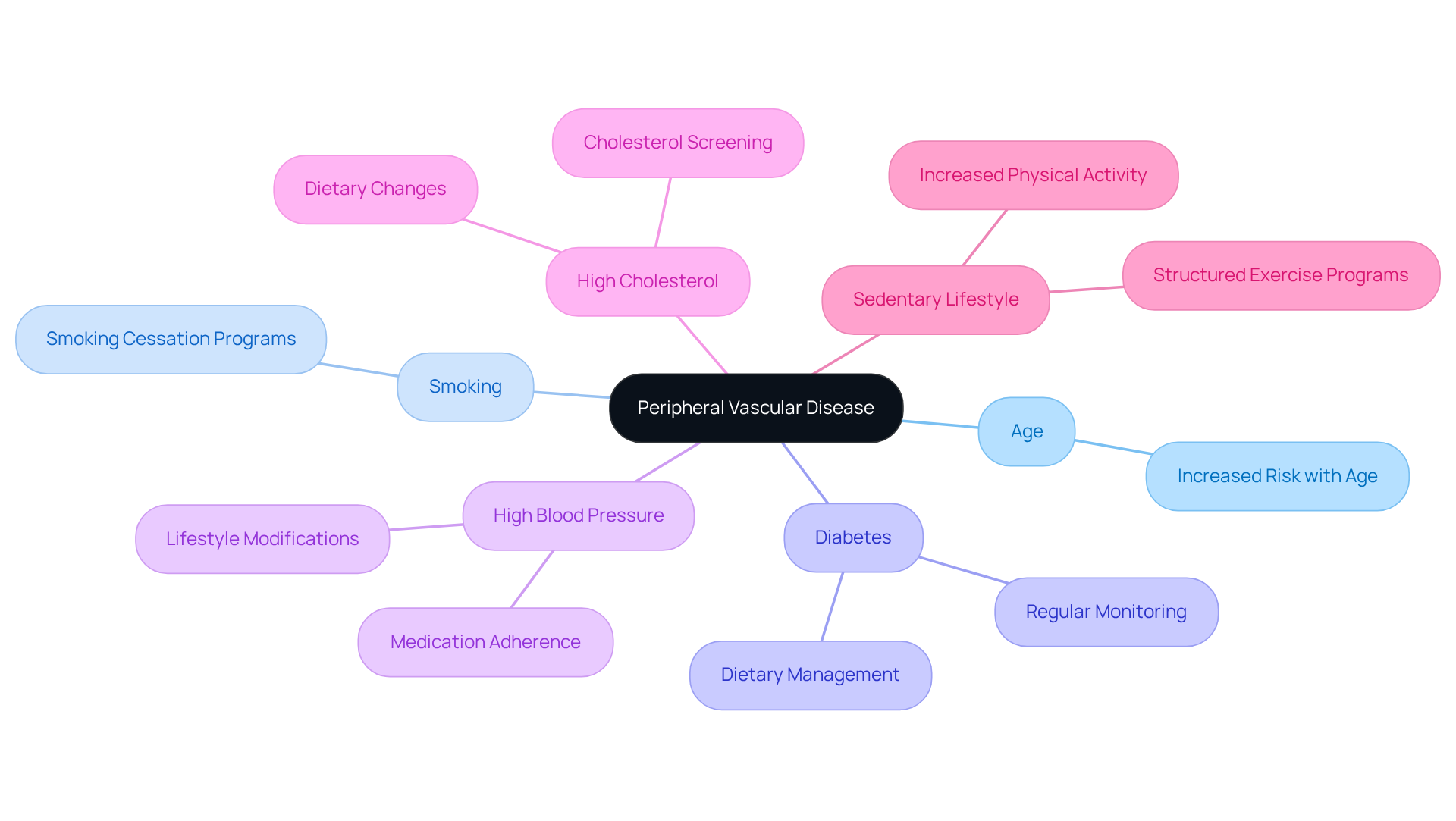
Several factors can contribute to the onset of peripheral vascular disease, including:
Understanding these factors is crucial, as it empowers individuals to take and seek the medical care they need. For those at higher risk, such as individuals with diabetes or hypertension, comprehensive evaluations and advanced imaging at Amavita Heart and Vascular Health offer targeted cardiovascular care. This specialized approach not only ensures effective monitoring and treatment but also addresses common heart concerns through advanced minimally invasive treatments tailored to each person's unique needs. Remember, you are not alone in this journey; we are here to support you every step of the way.
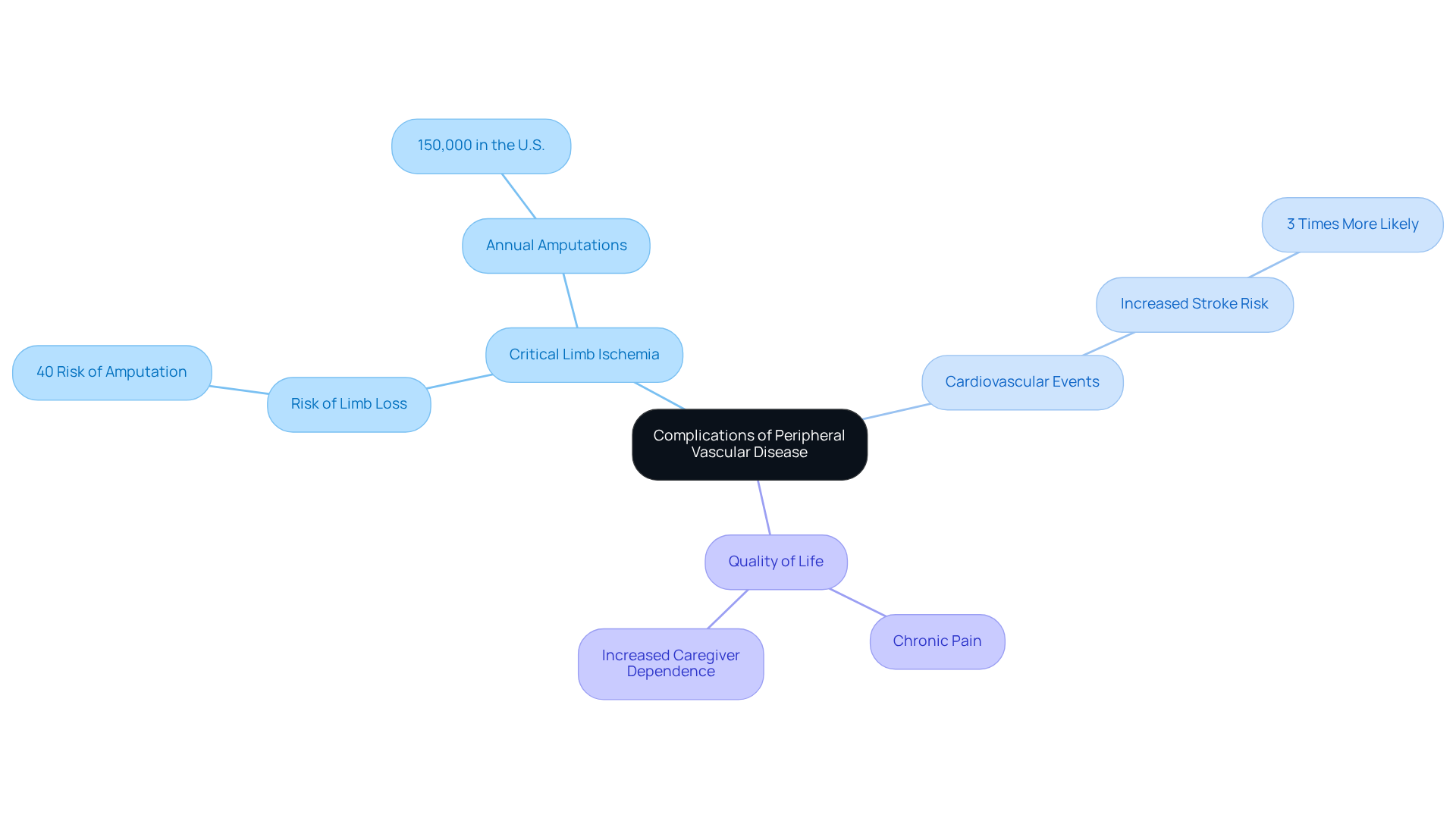
Untreated peripheral vascular disease poses significant health risks, including critical limb ischemia (CLI), which can lead to limb loss and an increased risk of cardiovascular events such as heart attacks and strokes. Each year, approximately 150,000 amputations occur in the U.S. due to complications from peripheral vascular disease, which underscores the urgent need for early intervention. Patients facing CLI face a daunting possibility of amputation; studies reveal that up to 40% of untreated cases may result in limb loss.
The consequences of CLI go beyond physical health; they can deeply affect one's quality of life, often resulting in chronic pain and increased reliance on caregivers. Vascular surgeons stress the importance of effectively managing PVD. Dr. Shuja notes, "Untreated PAD's greatest danger is limb loss, which leads to a loss of independence." This statement highlights the critical need for patients to actively participate in their treatment plans.
Moreover, the risk of cardiovascular events significantly escalates for those with peripheral vascular disease. Individuals with untreated peripheral artery conditions are three times more likely to experience a stroke, further emphasizing the importance of timely diagnosis and management. As the prevalence of peripheral vascular disease (PVD) continues to grow, particularly among older adults, understanding these challenges becomes essential for encouraging proactive healthcare choices and improving patient outcomes.
Have you considered discussing your vascular health with a healthcare provider? Your well-being is paramount, and taking the first step towards understanding your condition can lead to . Remember, you are not alone in this journey; there are resources and professionals ready to help you navigate your health concerns.
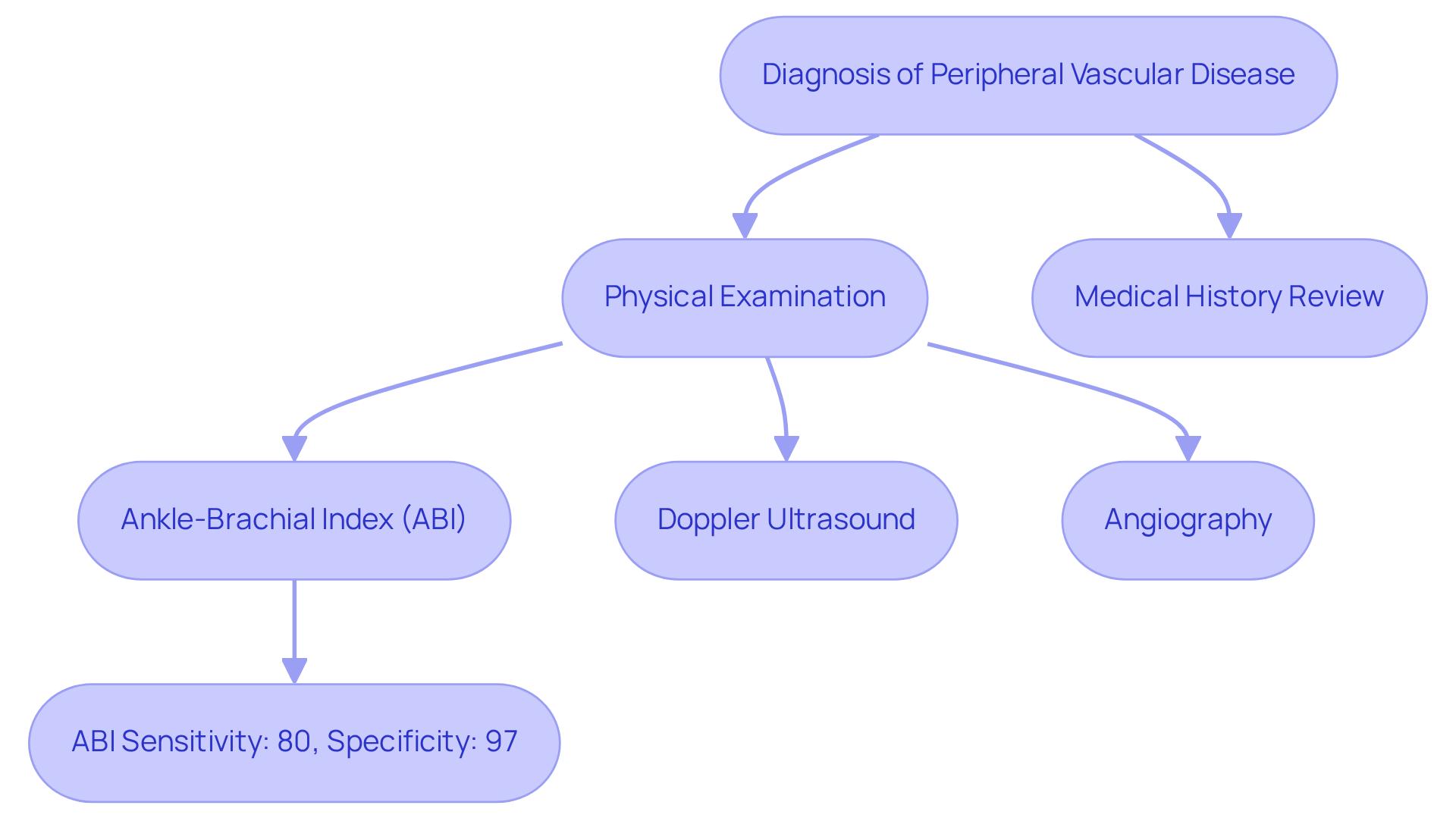
Diagnosing peripheral vascular disease is a crucial step in ensuring your health and well-being. It involves a thorough physical examination, a detailed review of your medical history, and specific diagnostic tests, such as the Ankle-Brachial Index (ABI), Doppler ultrasound, and angiography. The ABI test is particularly significant; it compares blood pressure readings in your ankle and arm to assess blood flow. Research indicates that an ABI score below 0.9 is a strong indicator of potential cardiovascular issues, with sensitivity rates reaching up to 80% and specificity rates of 97% for identifying peripheral vascular disease.
In addition to this, Doppler ultrasound complements the ABI by providing real-time images of blood flow in your arteries, allowing for the identification of any blockages or narrowing. Angiography, while more invasive, offers detailed visualization of blood vessels and is often used when more information is needed to guide your treatment decisions.
Real-world examples highlight the effectiveness of these diagnostic tools. For instance, a longitudinal study discovered that utilizing the lowest ankle blood pressure for ABI calculation identified 70% more individuals vulnerable to PVD compared to conventional methods. Cardiologists emphasize the importance of precise identification; as one remarked, 'The identification of peripheral vascular conditions can be adequately determined based on risk factors, clinical presentation, and physical examination results.' This underscores the significance of a thorough approach to , ensuring timely and effective management for individuals like you.
If you have concerns about your vascular health, please know that you are not alone. Seeking help is a vital step, and there are professionals ready to support you in understanding your condition and exploring your options for care.
At Amavita, we understand how challenging it can be to manage peripheral vascular disease. That’s why we offer a multifaceted approach that includes:
Our commitment to minimally invasive methods not only enhances your comfort but also promotes quicker recovery times and better results.
Research shows that have high success rates, particularly for older individuals. Many patients experience significant relief from symptoms and improved mobility after these procedures. In addition to this, leading cardiologists highlight that these techniques reduce the risks associated with traditional surgeries, making them a preferred choice for managing peripheral vascular disease.
By prioritizing these innovative treatments, Amavita ensures that you receive the highest standard of care tailored to your individual needs. We are here to support you every step of the way, helping you regain your quality of life with compassion and expertise. If you have any questions or concerns, please don’t hesitate to reach out to us—we’re here to help.
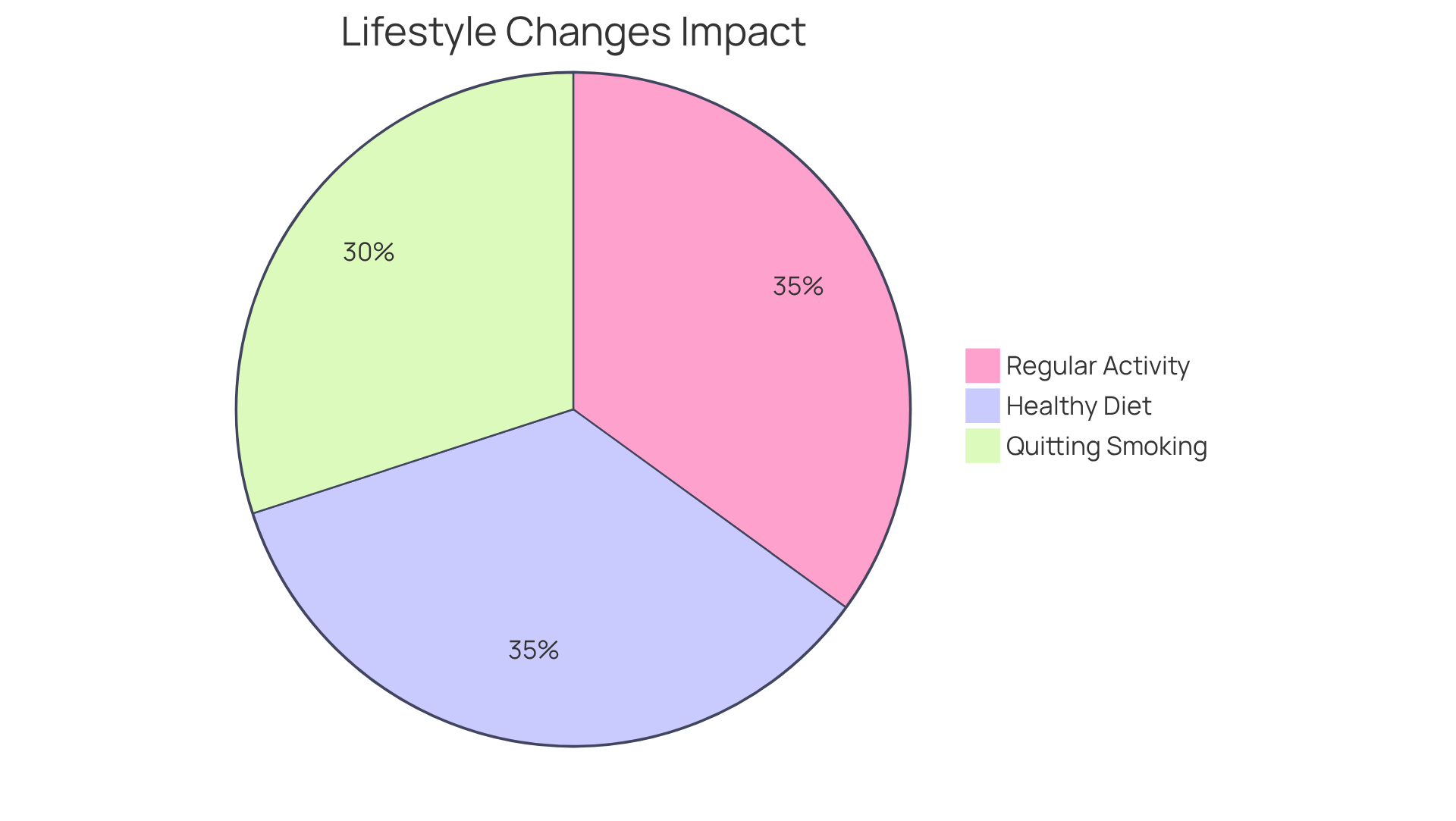
Effectively managing peripheral vascular disease requires embracing significant lifestyle changes. Have you considered how quitting smoking can be a crucial step? Tobacco use is a , and by taking this step, you can greatly improve your health. Engaging in regular physical activity, such as walking or structured exercise programs, can enhance blood flow and alleviate symptoms. Research shows that monitored exercise can lead to a 30% to 35% increase in walking distance for individuals suffering from peripheral vascular disease, which is truly encouraging.
A healthy diet is also essential in managing peripheral vascular disease. Focusing on fruits, vegetables, whole grains, and healthy fats—while steering clear of trans and saturated fats—can significantly improve your overall cardiovascular health. Nutritionists emphasize that a diet low in saturated fats can help reduce cholesterol levels, which is vital for individuals suffering from peripheral vascular disease. Many who adopt these dietary changes often report improved symptoms and a better quality of life, which is a comforting thought.
Statistics reveal that smoking cessation programs have a success rate of about 30% among older individuals, underscoring the potential for positive outcomes when support systems are in place. Additionally, the occurrence of peripheral artery condition (PAD) in individuals aged 50 and above ranges from 12% to 20%, highlighting the pressing need for these lifestyle modifications. Real-world examples show that those who commit to these changes not only manage their condition more effectively but also reduce their risk of severe complications, such as heart attacks and strokes. It’s important to note that over 150,000 amputations occur annually in the U.S. due to PAD, emphasizing the critical nature of effective management.
By prioritizing these essential lifestyle changes, you can significantly enhance your vascular health and overall well-being. Remember, you are not alone in this journey; support is available, and taking these steps can lead to a healthier, happier life.
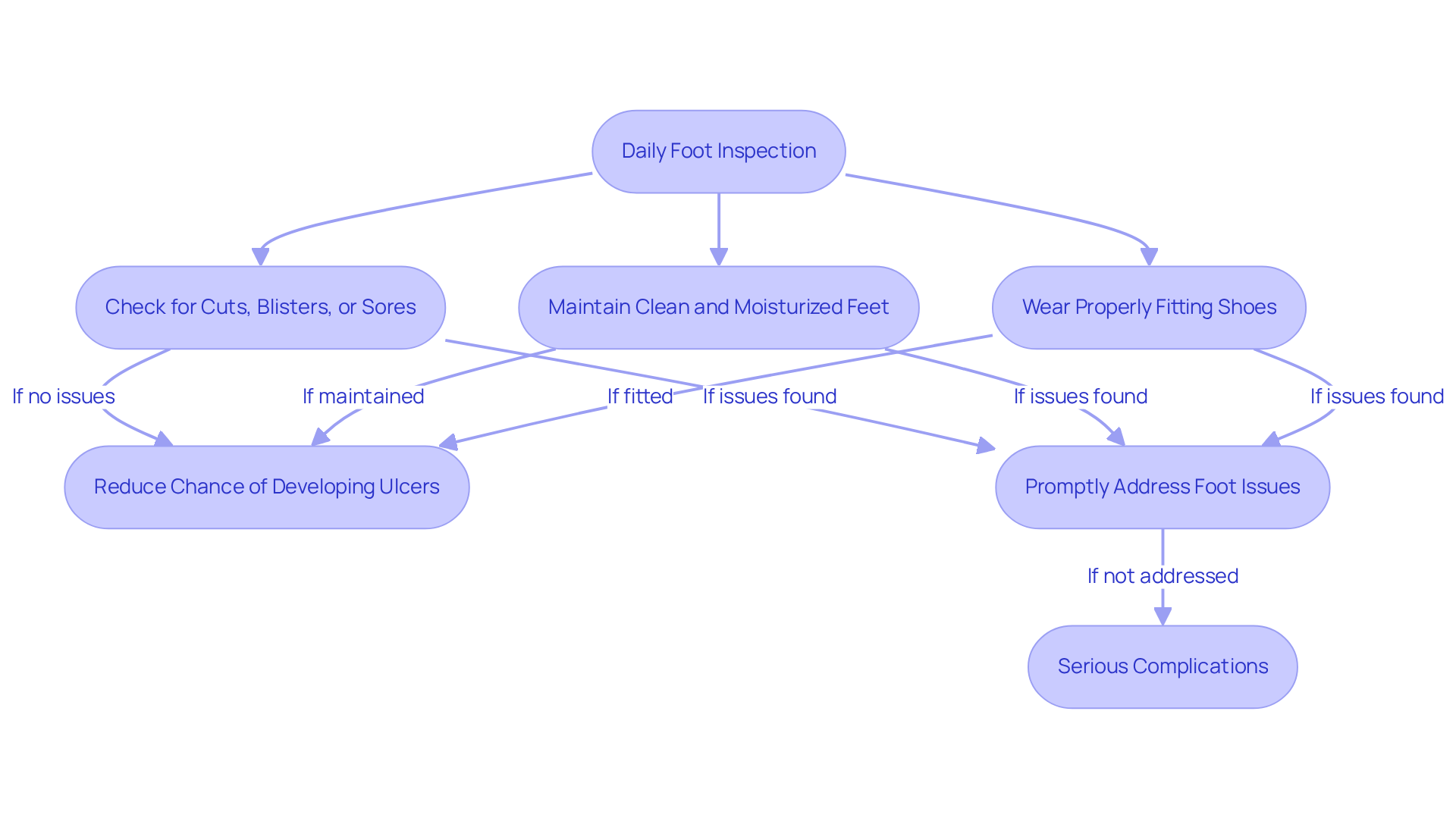
For individuals managing peripheral vascular disease, diligent foot care is essential to prevent serious complications. Regular foot inspections are crucial; patients should check for cuts, blisters, or sores daily. Maintaining clean and moisturized feet, along with wearing properly fitting shoes, can greatly decrease the chance of developing ulcers. In fact, diabetic foot ulcers occur in approximately 10% of people with diabetes, and the lifetime risk of developing one is as high as 25%.
Podiatrists emphasize that addressing foot issues promptly is vital. As Dr. David G. Armstrong notes, 'Early intervention can prevent minor problems from escalating into serious infections or amputations.' This is particularly important given that over 60% of in the U.S. are performed on individuals with diabetes, often stemming from untreated foot ulcers.
Furthermore, conditions like Peripheral Artery Disease (PAD) and Chronic Venous Insufficiency (CVI) can exacerbate foot health issues. At Amavita Heart and Vascular Health, our specialists utilize advanced diagnostic imaging to identify blockages in the arteries and provide minimally invasive treatments such as venous ablation, Varithena treatment, and sclerotherapy that restore blood flow, significantly improving mobility and reducing pain. For individuals experiencing symptoms of CVI, we provide outpatient procedures that can reduce swelling and discomfort, ensuring a comprehensive approach to foot care.
Real-life examples illustrate the effectiveness of these practices. For instance, an individual with peripheral vascular disease who adhered to a strict foot care regimen and sought expert treatment reported no complications over several years, highlighting the impact of proactive management.
Incorporating regular foot inspections into daily routines not only helps in identifying potential issues early but also fosters a sense of empowerment among patients. By prioritizing foot health and seeking expert treatment for underlying conditions related to peripheral vascular disease, individuals with PVD can significantly enhance their quality of life and lessen the chance of severe complications.
If you are experiencing severe leg pain, sudden changes in skin color, non-healing wounds, or signs of infection—like fever or increased redness—it’s very important to seek medical assistance promptly. These symptoms are critical indicators of worsening peripheral vascular disease and can lead to serious complications if they are not addressed. For example, untreated claudication can lead to a 1% annual chance of amputation, underscoring the urgency of recognizing these warning signs. Furthermore, non-healing wounds can become infected, significantly raising the risk of major amputation or limb loss. By recognizing these key signs, you can facilitate timely intervention, ultimately improving outcomes and preventing severe health consequences associated with peripheral vascular disease. As Dr. Charles C. Leithead emphasizes, early detection and management are vital to avoid the progression of peripheral vascular disease.
Key Signs to Watch For:
Action Steps:
Your health is important, and can make a significant difference in your care.

Understanding and managing peripheral vascular disease (PVD) is essential for maintaining your overall health and quality of life. The insights shared here highlight the importance of early detection, proactive lifestyle changes, and the advanced treatment options available through specialized care. By recognizing the symptoms and risk factors associated with PVD, you can take significant steps toward effective management and avoid severe complications.
Key arguments presented include the critical role of lifestyle modifications:
These vital changes not only improve your vascular health but also enhance your mobility and overall well-being. Furthermore, it’s crucial to prioritize regular foot care and monitoring, as neglecting these areas can lead to complications.
Ultimately, taking charge of your vascular health is a journey that requires awareness, education, and support. Seeking medical guidance and adhering to recommended lifestyle changes can lead to improved outcomes and a better quality of life. For those facing the challenges of peripheral vascular disease, remember that the available resources and expert care at facilities like Amavita Heart and Vascular Health can truly make a significant difference in managing this condition effectively.
What is peripheral vascular disease (PVD)?
Peripheral vascular disease is a condition that affects the blood vessels outside the heart and brain, primarily targeting the arteries in the legs. It involves the narrowing of blood vessels, which restricts blood flow and can lead to discomfort and pain, especially during physical activities like walking.
What are the main symptoms of peripheral vascular disease?
Key symptoms of peripheral vascular disease include leg pain or cramping during physical activities (intermittent claudication), numbness or weakness in the legs, coldness in the lower leg or foot, and non-healing sores or wounds. Notably, many individuals may have atypical symptoms that go unnoticed.
Why is it important to recognize the symptoms of PVD early?
Early recognition of PVD symptoms can lead to timely diagnosis and treatment, which significantly enhances quality of life. Early intervention can halt the progression of the condition and prevent serious complications, such as limb loss.
What are the major risk factors for developing peripheral vascular disease?
Major risk factors for peripheral vascular disease include smoking, diabetes, high blood pressure, and high cholesterol.
How does Amavita Heart and Vascular Health approach the treatment of peripheral vascular disease?
Amavita Heart and Vascular Health focuses on providing exceptional treatment through minimally invasive techniques, such as venous ablation for varicose veins, and comprehensive diagnostic testing. This approach enhances patient comfort and reduces recovery times.
What advantages do minimally invasive techniques offer for PVD treatment?
Minimally invasive techniques allow individuals to return to daily activities more quickly and minimize the risks associated with traditional surgical procedures.
What is the projected prevalence of peripheral vascular disease among older adults by 2050?
By 2050, the prevalence of peripheral vascular disease is projected to exceed 21% in women and 14% in men over age 65.
How can lifestyle modifications impact peripheral vascular disease?
Lifestyle modifications, such as smoking cessation and increased physical activity, have proven effective in managing early-stage peripheral vascular disease and can significantly reduce associated risks.
What role do healthcare professionals play in managing peripheral vascular disease?
Healthcare professionals emphasize the importance of routine check-ups and discussions with primary care physicians to manage peripheral vascular disease effectively and prevent serious complications.
Is support available for individuals dealing with peripheral vascular disease?
Yes, support is available for individuals navigating their health concerns related to peripheral vascular disease, helping them take meaningful steps to manage their cardiovascular health.