


This article serves as a compassionate guide for treating Deep Vein Thrombosis (DVT) in elderly patients. It emphasizes the critical role of anticoagulation therapy, lifestyle changes, and vigilant monitoring for complications. Are you or a loved one concerned about DVT? Understanding these treatment options, such as anticoagulants and compression stockings, can be reassuring.
Moreover, it highlights the necessity of personalized care strategies and proactive management to mitigate risks associated with DVT and its potential complications, especially in older adults.
Remember, you are not alone in this journey—support is available to help you navigate these challenges.
Understanding Deep Vein Thrombosis (DVT) is crucial, particularly for the elderly, who face an increased risk due to various health factors. This guide offers a comprehensive overview of treatment options, highlighting the importance of timely intervention and personalized care strategies to help mitigate complications. With so many treatment avenues available, caregivers and patients may wonder: how can they ensure they are choosing the most effective approach tailored to individual needs?
In addition to this, it’s essential to recognize that every patient is unique, and what works for one person may not work for another. By exploring various treatment options, we can find solutions that resonate with the specific needs of each individual. Furthermore, reaching out for support can make a significant difference in navigating these choices. Remember, you are not alone in this journey, and there are compassionate professionals ready to assist you every step of the way.
Deep Vein Thrombosis (DVT) is a serious condition characterized by the formation of a clot in a deep vein, most often in the legs. Symptoms may include swelling, pain, redness, and warmth in the affected area, but sometimes DVT can occur without any noticeable symptoms. This makes and intervention. Elderly patients face heightened risks due to various factors, including:
Recent studies indicate that more than one-third of venous thromboembolism (VTE) cases are linked to recent hospitalizations, underscoring the importance of vigilant monitoring during and after hospital stays. Moreover, as many as 70% of healthcare-associated VTE cases are preventable through measures such as anticoagulant medications or compression stockings. The likelihood of developing DVT significantly increases with hospitalization for major illnesses and surgical interventions, particularly among older adults.
Recognizing these signs and understanding the associated risk factors can lead to timely medical intervention, significantly reducing the risk of severe complications like pulmonary embolism, which can be life-threatening. It’s also important to note that one third to one half of individuals who have had a DVT will face long-term complications known as post-thrombotic syndrome, which can include symptoms such as swelling, pain, discoloration, and scaling in the affected limb.
A multidisciplinary approach that considers the unique physiological and functional diversity of older individuals, including addressing frailty, comorbidity burden, and polypharmacy, is essential for effective management and improved outcomes. At Amavita Heart and Vascular Health, we emphasize comprehensive management of Chronic Venous Insufficiency and Advanced Vascular Disease, recognizing their impact on DVT. Our shared decision-making process aligns interventions with patient-specific goals, ensuring that elderly patients receive personalized care tailored to their vascular health needs.

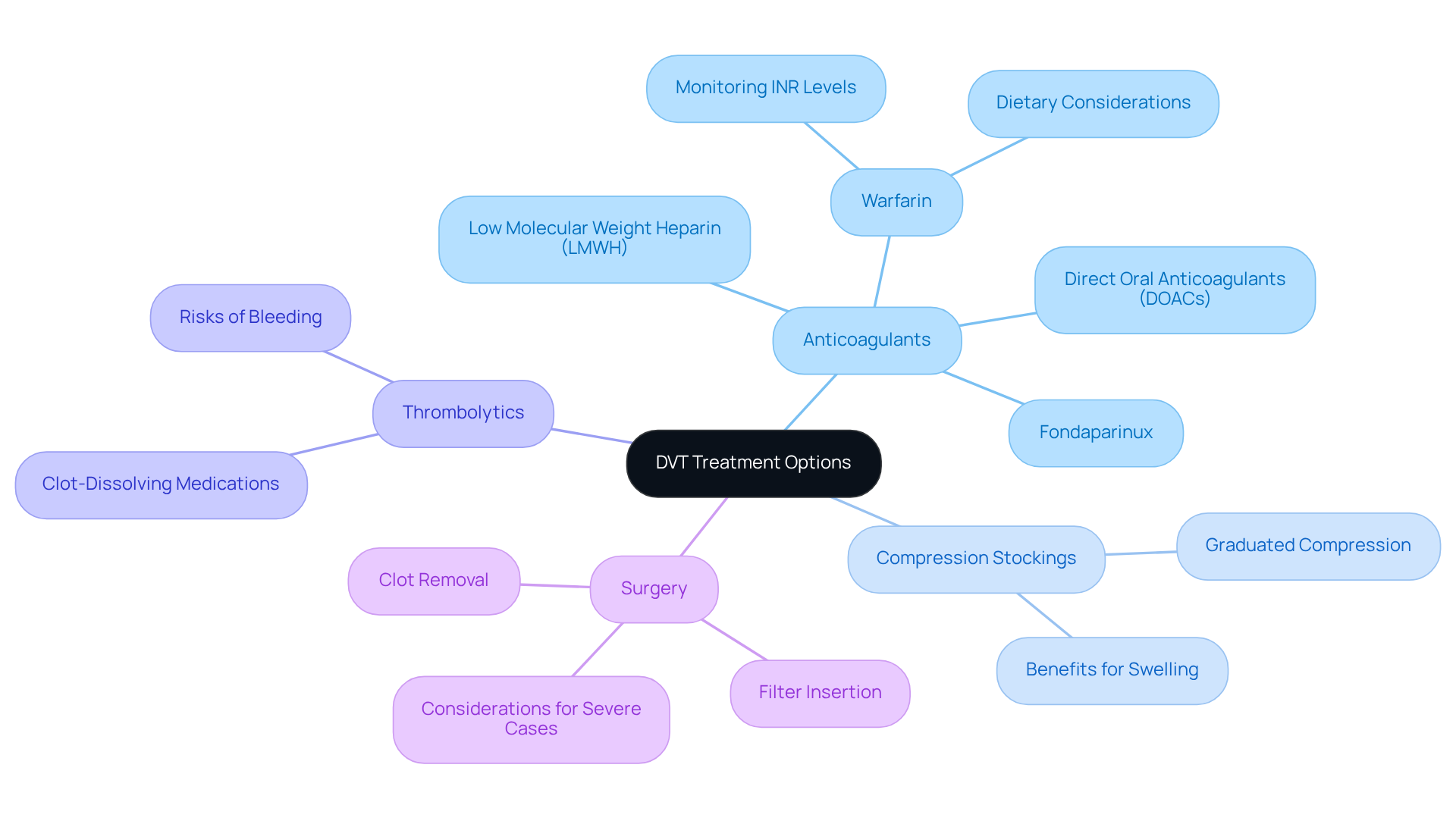
Understanding how to treat DVT involves management strategies that focus on stopping clot development and reducing the risk of pulmonary embolism. Understanding your options is essential, and we are here to support you every step of the way.
It’s important to discuss how to treat DVT among each treatment option thoroughly with your healthcare provider to determine the best approach for your unique health situation. Vascular specialists emphasize the importance of personalized treatment strategies, particularly for older individuals who might face specific risks associated with anticoagulation therapy. Recent advancements in anticoagulants, including fixed-dose options that do not require regular testing, are expected to improve adherence and enhance your quality of life. Remember, you are not alone in this journey; we are here to help you navigate your care.
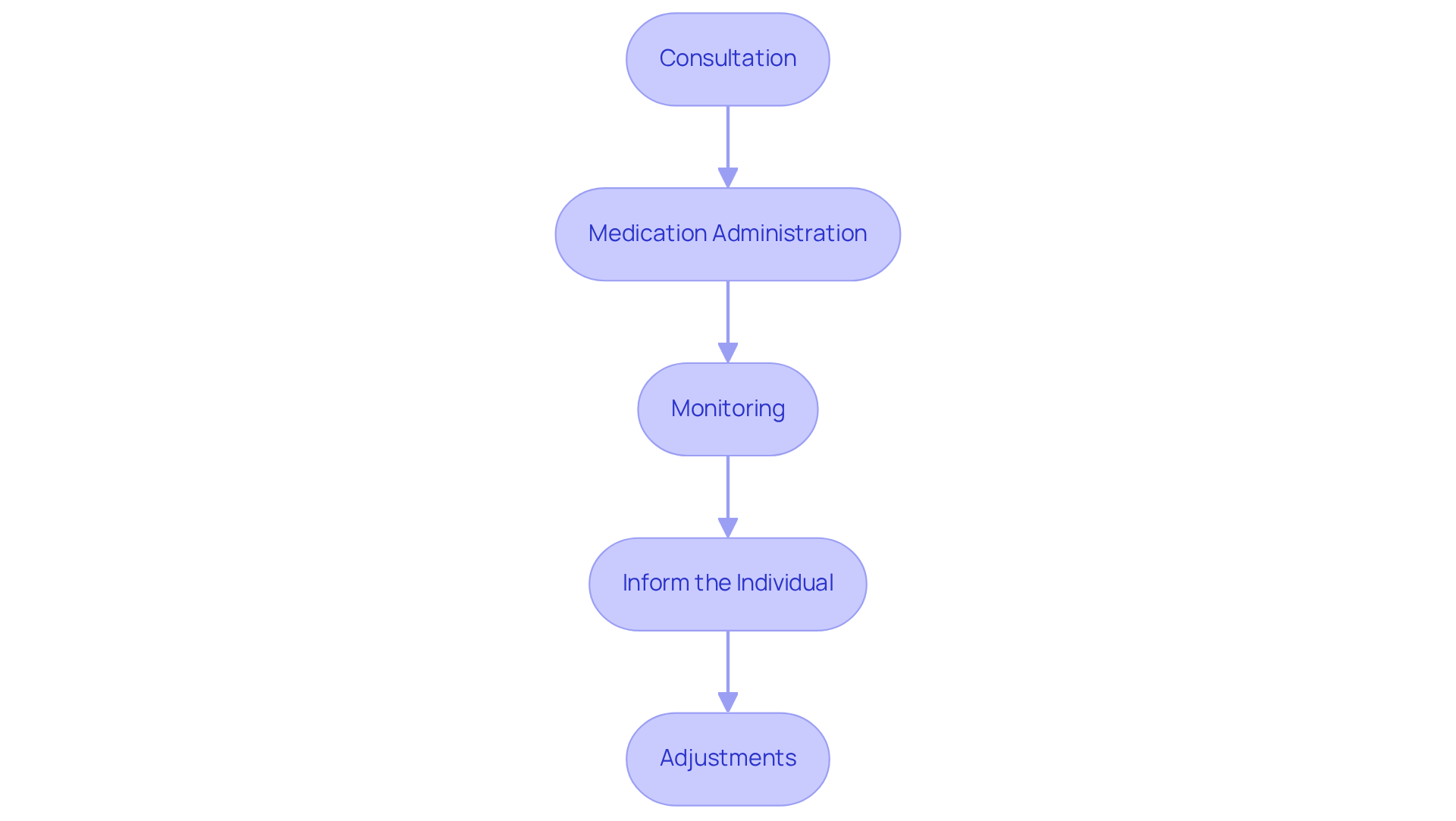
Administering anticoagulation therapy involves several key steps that can make a significant difference in your care:
By following these steps, caregivers can help ensure that individuals receive the full benefits of anticoagulation therapy while minimizing risks. This structured method not only improves safety for individuals but also aligns with the latest recommendations for managing anticoagulation in older adults. Furthermore, emerging trends such as the development of factor XIa inhibitors and the integration of AI in monitoring can further enhance patient outcomes. Remember, you are not alone in this journey; support is always available to help you navigate your treatment.
Lifestyle changes and self-care strategies are vital for understanding how to treat DVT and preventing its recurrence. Here are some key recommendations to consider:
By incorporating these lifestyle modifications into your everyday habits, you can greatly lower your chances of DVT recurrence and understand how to treat DVT, which will improve your overall cardiovascular well-being. Regular follow-ups with healthcare providers are also essential to monitor your progress and adjust treatment plans as necessary. Furthermore, recognizing the signs of clots and seeking timely medical care can help avert complications such as pulmonary embolism or stroke. Remember, you are not alone in this journey, and support is always available.

Monitoring for complications is an essential part of managing deep vein thrombosis (DVT), especially for our elderly patients who may face serious risks like pulmonary embolism (PE). It’s important for caregivers and healthcare providers to stay alert for these key indicators:
By taking a proactive approach to monitoring and adjusting treatment, caregivers can greatly improve the chances of positive outcomes for patients who are learning how to treat DVT. Given the notably high incidence of pulmonary embolism among seniors, knowing how to treat DVT is crucial for effective management and timely intervention. Remember, you are not alone in this journey; support is always available.

Understanding and effectively managing Deep Vein Thrombosis (DVT) in elderly patients is crucial for preventing serious complications and ensuring a better quality of life. Recognizing risk factors, symptoms, and tailored treatment options is essential for older adults. By prioritizing awareness and timely intervention, caregivers and healthcare providers can significantly reduce the risks associated with this condition.
Key insights include:
Monitoring for complications and adjusting treatment plans based on individual responses are vital steps in providing comprehensive care. A multidisciplinary approach ensures that elderly patients receive personalized management strategies that align with their unique health needs.
Ultimately, the journey of treating DVT does not have to be faced alone. Empowering patients and caregivers through education, support, and proactive health management can lead to improved outcomes and enhanced overall well-being. It is essential to remain vigilant about the signs of complications and to maintain open communication with healthcare providers to navigate this complex condition effectively. Taking these steps not only aids in the treatment of DVT but also fosters a healthier, more active lifestyle for elderly individuals.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a serious condition characterized by the formation of a clot in a deep vein, most commonly in the legs. Symptoms may include swelling, pain, redness, and warmth in the affected area, but DVT can also occur without noticeable symptoms.
Who is at higher risk for developing DVT?
Elderly patients, particularly those over 60, are at heightened risk for DVT due to factors such as prolonged immobility, recent surgery or injury, chronic medical conditions (including cancer and heart disease), and a family history of blood clots.
How common are DVT cases associated with hospitalizations?
More than one-third of venous thromboembolism (VTE) cases are linked to recent hospitalizations, highlighting the importance of monitoring during and after hospital stays.
Can DVT lead to serious complications?
Yes, DVT can lead to severe complications such as pulmonary embolism, which can be life-threatening. Additionally, one-third to one-half of individuals who have had a DVT may experience long-term complications known as post-thrombotic syndrome.
What are the treatment options for DVT?
Treatment options for DVT include: - Anticoagulants: Medications like low molecular weight heparin (LMWH), fondaparinux, and direct oral anticoagulants (DOACs) to thin the blood and prevent further clotting. - Compression stockings: Designed to alleviate swelling and improve blood flow in the legs. - Thrombolytics: Clot-dissolving medications used in severe cases, but carry a higher risk of bleeding. - Surgery: Rarely necessary, but may be required to remove a clot or insert a filter to prevent clots from reaching the lungs.
Why is careful monitoring important for elderly patients receiving anticoagulants?
Elderly patients are at a higher risk of bleeding, and managing their therapeutic range for INR can be more complex, making careful monitoring essential.
What role does a multidisciplinary approach play in DVT management?
A multidisciplinary approach considers the unique physiological and functional diversity of older individuals, addressing factors like frailty and comorbidity burden to ensure effective management and improved outcomes.
How can patients ensure they receive personalized care for DVT?
Patients should engage in a shared decision-making process with their healthcare providers to align interventions with their specific goals and health needs, ensuring personalized care tailored to their vascular health.