Deep Vein Thrombosis, commonly known as DVT, can be a concerning condition, especially for elderly patients. It's primarily treated with anticoagulant medications like heparin, warfarin, and direct oral anticoagulants (DOACs). These medications play a vital role in preventing further clotting and reducing the risk of serious complications, such as pulmonary embolism.
In addition to medication, it's essential to understand the importance of adhering to treatment plans, attending regular follow-ups, and making lifestyle modifications. These steps can significantly help in managing and preventing future episodes of DVT. For elderly patients, who may be at a higher risk, these measures are crucial.
We encourage you to take these recommendations to heart, as they can lead to better health outcomes. Remember, you are not alone in this journey; support is available, and taking proactive steps can make a difference in your quality of life.
Deep Vein Thrombosis (DVT) represents a serious health concern, especially for the elderly, whose unique vulnerabilities can lead to significant complications if not addressed promptly. This article aims to provide a compassionate guide, shedding light on the treatment options available for older patients facing this condition.
Yet, the path to effective management can be challenging—how can caregivers and patients feel empowered with the right knowledge and resources to tackle DVT effectively?
By delving into the nuances of DVT treatment, readers will discover essential strategies that not only address immediate worries but also lay the foundation for long-term health and well-being.
Deep Vein Thrombosis (DVT) is a serious condition that involves the formation of a blood clot in a deep vein, most often in the legs. This condition can pose significant risks, particularly for older patients, who may face complications like pulmonary embolism if the clot dislodges and travels to the lungs. Factors that increase the likelihood of DVT in older adults include:
Understanding DVT is essential, especially since studies show that elderly individuals are particularly at risk for its complications. For example, nearly one-third to one-half of those who have experienced a DVT may endure long-term complications, such as post-thrombotic syndrome, which can lead to swelling, pain, and discoloration in the affected limb. Additionally, the risk of recurrence is notable, with approximately 33% of individuals experiencing another event within ten years.
Recent studies underscore the importance of DVT awareness initiatives, which have proven to enhance health outcomes for older individuals. These initiatives aim to educate both patients and healthcare providers about the signs of DVT, promoting early intervention and preventive measures. Cardiologists stress that recognizing and managing DVT in a timely manner can greatly diminish the risk of severe complications, making awareness and education crucial components of care for older adults.
If you or a loved one are concerned about DVT, remember that seeking help is a vital step. There are resources and support available to guide you through understanding this condition better, ensuring you receive the care you need. Your matter, and taking action can lead to a healthier future.

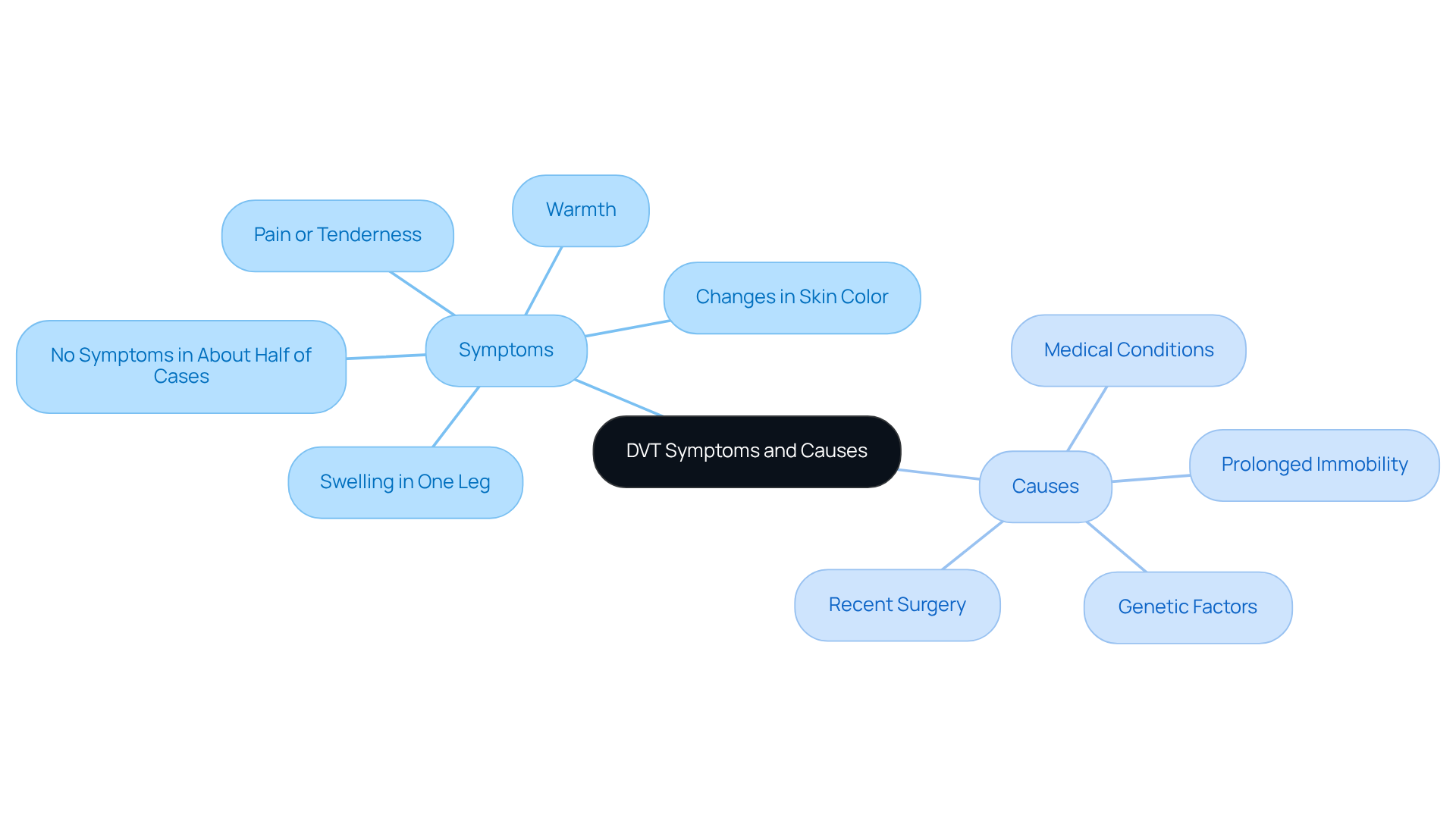
Deep vein thrombosis (DVT) can manifest through common signs such as:
However, it’s important to note that about half of those with DVT may not experience any symptoms at all. This makes , particularly for our elderly patients. Prolonged immobility, recent surgery, certain medical conditions like cancer or heart disease, and genetic factors can all contribute to the development of DVT in older adults. Research indicates that as we age, especially after 40, the likelihood of blood clots increases significantly. Additionally, conditions such as obesity and a history of blood clots further elevate this risk.
Geriatric experts emphasize the importance of recognizing these signs early. Prompt medical action can help prevent severe complications, such as pulmonary embolism and post-thrombotic syndrome, which may lead to long-term issues. Furthermore, signs like swelling, pain, or visible veins in the legs could suggest Chronic Venous Insufficiency (CVI), a condition where blood accumulates in the legs due to valve dysfunction. If left unaddressed, this can worsen throughout the day and potentially lead to skin ulcers.
At Amavita Heart and Vascular Health, we are dedicated to providing comprehensive vascular assessments and minimally invasive treatments to manage CVI and enhance circulation. It’s crucial for caregivers and individuals to be aware of these factors and to reach out to their doctor promptly to understand how DVT is treated if they notice any signs of the condition. Remember, you are not alone in this journey; we are here to support you every step of the way.
Diagnosing deep vein thrombosis (DVT) requires a thoughtful evaluation that combines physical examinations with specific diagnostic tests. One essential tool in this process is the Wells Score, which helps assess the likelihood of DVT based on an individual’s symptoms and contributing factors. This scoring system is particularly beneficial for older adults, as it takes into account age-related factors that may influence the risk of DVT.
Common diagnostic tests used alongside the Wells Score include:
The Wells Score has demonstrated high accuracy in diagnosing DVT, with studies indicating that it can effectively stratify risk in older individuals. For example, research suggests that the Wells Score can reliably predict DVT in approximately 80% of cases among older individuals. Vascular specialists highlight its significance, noting that a higher score correlates with an increased likelihood of DVT. Dr. Kahn, a respected researcher in vascular health, shares, "In individuals with acute DVT, early walking exercise is safe and may assist in alleviating acute issues," underscoring the importance of timely diagnosis and intervention.
Understanding these empowers patients and caregivers to engage more effectively with healthcare providers, ensuring timely and appropriate care. Additionally, preparing for DVT appointments by listing symptoms, personal health information, and questions can facilitate better communication and enhance the overall healthcare experience. Remember, you are not alone in this journey, and seeking help is a positive step towards better health.

A crucial aspect of managing deep vein thrombosis (DVT) is understanding how DVT is treated, primarily involving anticoagulant drugs that prevent further clotting and reduce the risk of pulmonary embolism. Understanding how DVT is treated can feel overwhelming, but rest assured, there are effective solutions available.
Many hematologists highlight that DOACs offer significant benefits for seniors, simplifying management and reducing the frequency of blood tests. Studies show that these medications are as effective as traditional anticoagulants like warfarin, with lower rates of major bleeding complications. For context, understanding how DVT is treated includes the average duration of treatment with low-molecular-weight heparins, which is 7-14 days and is important for your treatment timeline.
In more severe cases, thrombolytic therapy may be an option to dissolve clots. This approach is typically reserved for individuals experiencing significant limb ischemia or those at high risk for complications. While success rates for how DVT is treated can vary, recent data suggests that DOACs have shown promising results, with many patients reporting relief and an improved quality of life.
A systematic review by Kahn et al. found that engaging in early walking exercises is safe and may help alleviate acute symptoms, underscoring the importance of your involvement in your treatment plan. Have you considered discussing your options with your healthcare provider? It’s essential to explore how DVT is treated while considering the most appropriate treatments tailored to your overall health and any other medications you may be taking.
Success stories from older adults who have been treated with DOACs highlight the potential for effective DVT management. Many individuals have been able to maintain an active lifestyle while minimizing the risks associated with this condition. Remember, you are not alone in this journey—support is available, and you deserve to feel empowered in managing your health.

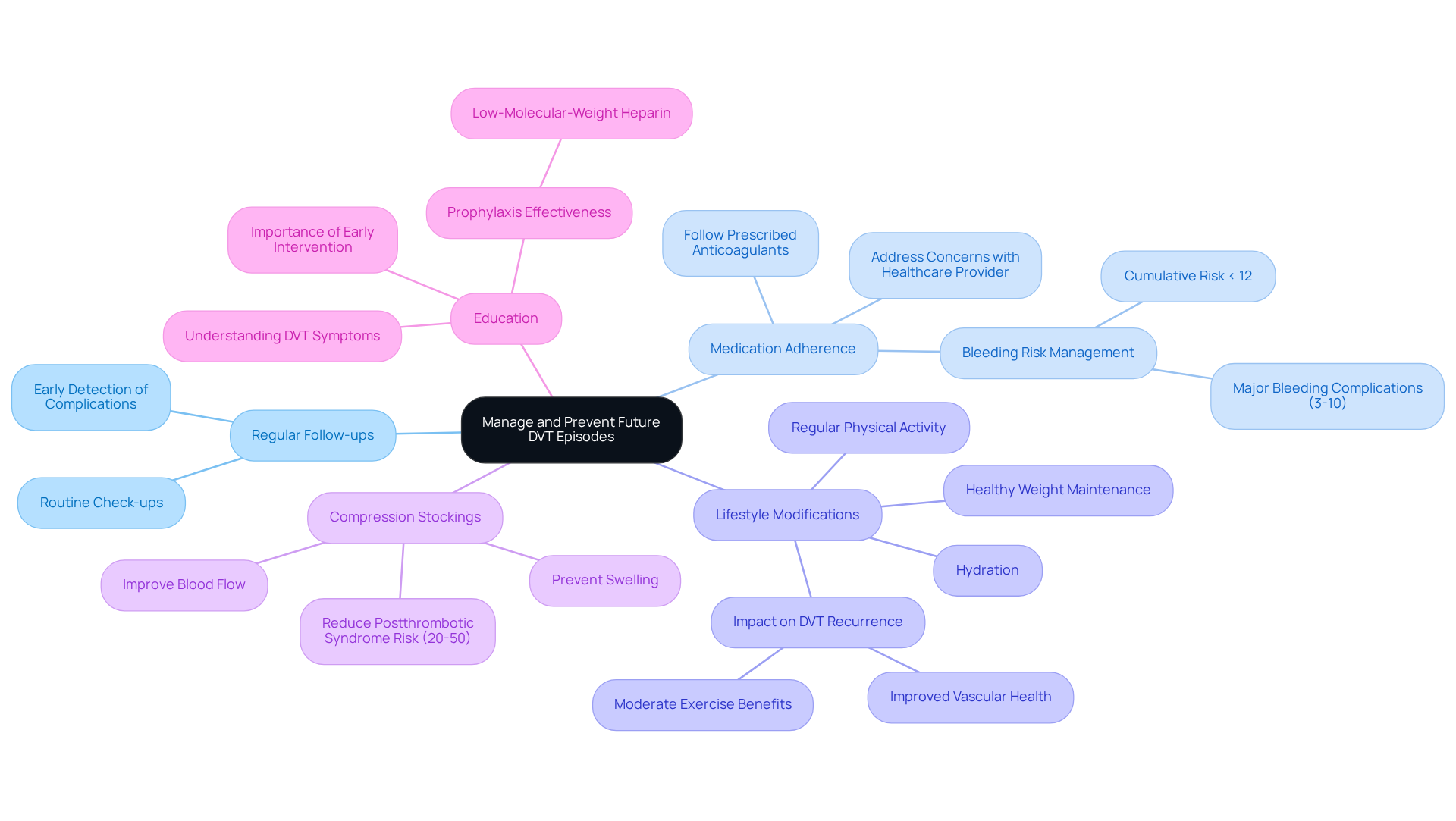
To effectively manage and prevent future episodes of deep vein thrombosis (DVT), elderly patients are encouraged to consider the following compassionate strategies:
By implementing these strategies, elderly patients can significantly reduce their risk of recurrent DVT and understand how DVT is treated to enhance their overall cardiovascular health. Remember, you are taking important steps towards a healthier future, and support is always available.
Understanding and managing Deep Vein Thrombosis (DVT) is crucial, especially for elderly patients who face heightened risks and complications from this condition. It’s important to be aware of the potential dangers, and timely diagnosis along with effective treatment strategies can truly make a difference. By educating both patients and caregivers about the symptoms, causes, and available treatments, individuals can take proactive steps towards safeguarding their health.
Key insights discussed include:
Ultimately, empowering elderly patients with knowledge and resources is vital for enhancing their quality of life and preventing future DVT episodes. It is essential to engage in open conversations with healthcare providers and stay informed about the latest treatment advancements. By adopting a proactive approach to health management, patients can foster better health outcomes. Taking these steps not only cultivates a sense of control over one’s well-being but also ensures that elderly individuals can lead active, fulfilling lives while minimizing the risks associated with DVT.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a serious condition characterized by the formation of a blood clot in a deep vein, most commonly in the legs. It poses significant risks, especially for older patients, as it can lead to complications like pulmonary embolism if the clot dislodges and travels to the lungs.
Who is at higher risk for developing DVT?
Older adults are at higher risk for developing DVT due to factors such as reduced mobility, chronic health conditions, and certain medications that increase susceptibility to clot formation.
What are the potential long-term complications of DVT?
Long-term complications of DVT can include post-thrombotic syndrome, which may cause swelling, pain, and discoloration in the affected limb. There is also a notable risk of recurrence, with approximately 33% of individuals experiencing another DVT event within ten years.
What symptoms should one look for in DVT?
Common symptoms of DVT include swelling in one leg, pain or tenderness, warmth, and changes in skin color. However, about half of those with DVT may not experience any symptoms at all.
What factors contribute to the development of DVT in older adults?
Contributing factors for DVT in older adults include prolonged immobility, recent surgery, certain medical conditions (like cancer or heart disease), genetic factors, obesity, and a history of blood clots.
Why is early recognition of DVT symptoms important?
Early recognition of DVT symptoms is crucial because prompt medical action can prevent severe complications, such as pulmonary embolism and post-thrombotic syndrome, which may lead to long-term health issues.
What should individuals do if they notice signs of DVT?
Individuals who notice signs of DVT should reach out to their doctor promptly to understand how DVT is treated. Seeking help is vital for managing the condition and ensuring proper care.
What resources are available for those concerned about DVT?
There are resources and support available to help individuals and their loved ones understand DVT better and navigate their care. It is important to take action for health and well-being.