


Blood clots in the leg can be concerning, but there are effective treatments available that can help. These include:
Each of these treatments plays a vital role in preventing clot enlargement, dissolving existing clots, and improving circulation. It's essential to seek timely medical attention, as this can significantly reduce the risk of complications, such as pulmonary embolism. Remember, you are not alone in this; there are caring professionals ready to support you every step of the way.
Understanding the complexities of blood clots in the leg is crucial, especially considering their potential to lead to serious health complications. This guide gently explores the various treatment options available, offering essential insights into how to effectively manage and prevent these potentially life-threatening conditions.
With so many treatment pathways and preventive measures, you may wonder how to discern the best course of action for your specific situation. This article aims to unravel these complexities, providing a step-by-step approach to understanding and treating blood clots in the leg, ensuring you feel supported every step of the way.
Thrombi, or coagulated fluid, can form when blood thickens and clumps together, often due to injury or prolonged immobility. Understanding the can help you take proactive steps to protect your health.
Immobility: Have you ever noticed how sitting for long periods, like during a flight or while resting in bed, can slow blood flow? This can significantly increase the risk of clot formation. Studies show that over one-third of venous thromboembolism (VTE) cases diagnosed each year are linked to recent hospital stays, with many occurring after discharge. Cardiologists emphasize the importance of staying active, especially for the elderly, to help reduce the risk of thrombus formation.
Surgery: Surgical procedures, particularly those involving the legs or pelvis, can damage veins and raise the risk of clotting. For instance, VTE is a leading cause of preventable hospital death in the United States, particularly after surgeries like total hip or knee joint replacements. If you or a loved one are facing surgery, it’s vital to discuss these risks with your healthcare provider.
Medical Conditions: Certain health issues, such as cancer and heart disease, can make individuals more susceptible to blood clots. Research indicates that up to 60% of cancer patients may die from clots rather than the cancer itself, highlighting the need for careful monitoring in this group. Additionally, one-third to one-half of individuals with deep vein thrombosis (DVT) may face long-term complications, including swelling, pain, discoloration, and scaling in the affected limb.
Hormonal Factors: Hormonal changes, such as those during pregnancy or from birth control pills, can also increase the likelihood of clotting. Did you know that women are five times more likely to experience a VTE during pregnancy, childbirth, or in the three months following delivery?
Risk Factors:
Recognizing these factors is crucial for understanding your personal risk and taking steps toward prevention and treatment. It's reassuring to know that as many as 70% of healthcare-associated VTE cases can be prevented through measures such as anticoagulant medications or compression stockings, which relates to how blood clots in the leg are treated. By being aware of these risks and preventive strategies, you can better manage your health and well-being.

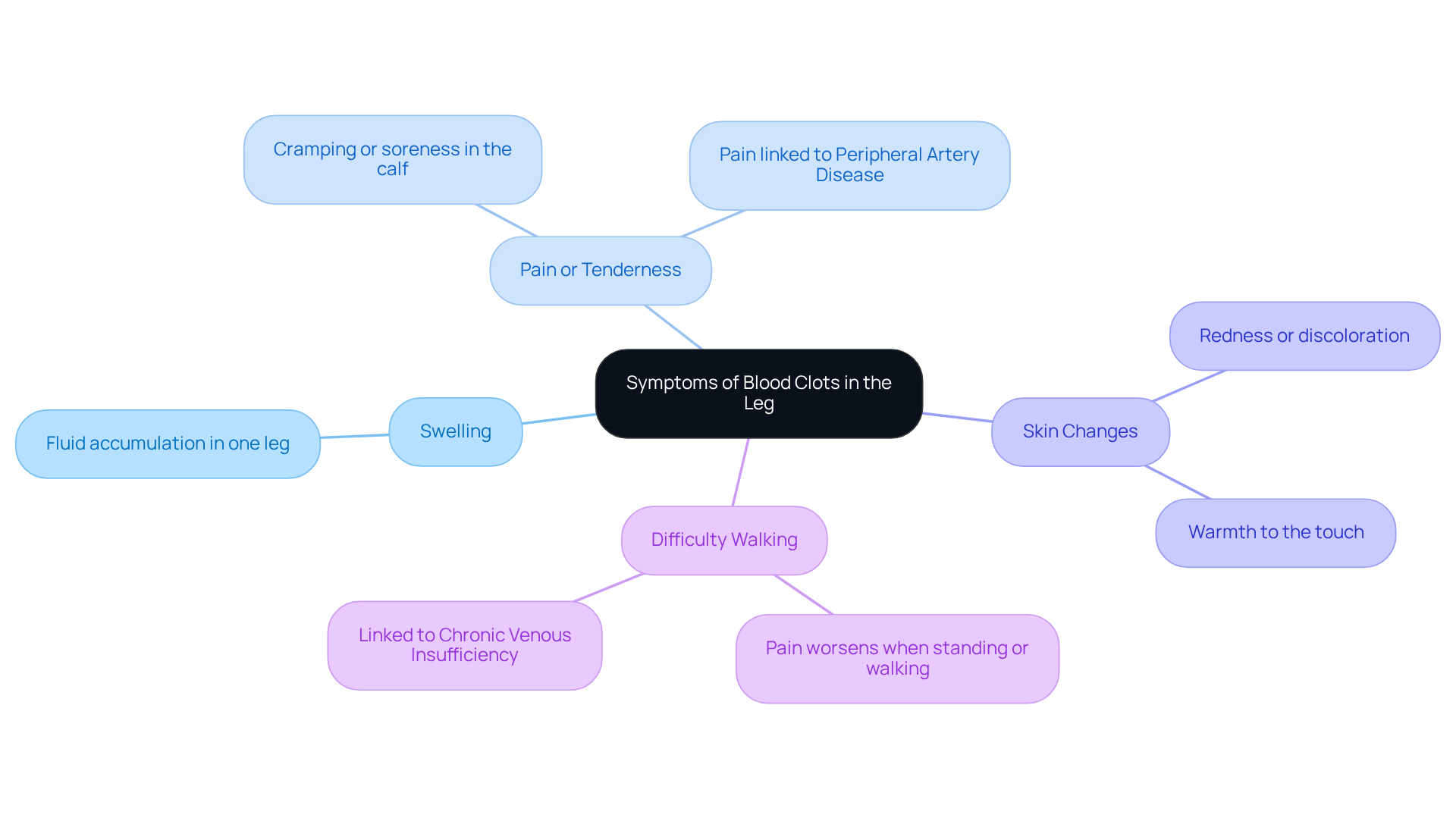
Indicators of vascular blockages in the leg, particularly deep vein thrombosis (DVT), can manifest in various ways, leading to serious complications if not addressed promptly, which raises concerns about how are blood clots in leg treated. It’s essential to be aware of these key indicators:
It’s important to recognize that up to 30-40% of DVT cases can be asymptomatic, highlighting the need for vigilance. If you experience these symptoms suddenly, please seek medical attention immediately to understand how are blood clots in leg treated. At Amavita Heart and Vascular Health, our specialists are dedicated to utilizing advanced diagnostic imaging to identify blockages and explain how are blood clots in leg treated, including expert treatment options like minimally invasive procedures such as venous ablation, Varithena treatment, and sclerotherapy. Prompt identification and treatment can significantly reduce the risk of complications, such as the serious condition of pulmonary embolism, which can occur when considering how are blood clots in leg treated, especially when a thrombus travels to the lungs. Remember, timely intervention is crucial in understanding how are blood clots in leg treated, as it can lower the likelihood of mortality from untreated DVT from approximately 30% to between 2-8%. Additionally, maintaining a healthy weight and staying active are vital lifestyle changes that can help prevent DVT. Ignoring these symptoms can lead to serious complications, such as post-thrombotic syndrome, which affects many DVT patients and raises the question of how are blood clots in leg treated. Therefore, recognizing symptoms and seeking is crucial.
To understand how blood clots in the leg are treated, it is important to know that the treatment often involves a multifaceted approach, combining medications and, when necessary, procedures to ensure optimal outcomes.
Moreover, conditions like Chronic Venous Insufficiency (CVI) and Peripheral Artery Disease (PAD) can complicate the management of thrombosis. At Amavita Heart and Vascular Health, our specialists utilize advanced diagnostic imaging to identify underlying issues and offer minimally invasive treatments for CVI, such as venous ablation and sclerotherapy, which can alleviate symptoms and enhance overall leg health.
Engaging in a thorough discussion with your healthcare provider about how blood clots in the leg are treated is crucial to determine the most suitable course of action tailored to your individual health needs and circumstances. Furthermore, considering lifestyle changes and understanding the costs associated with treatment can play a vital role in managing your condition effectively. Remember, you are not alone in this journey, and support is always available.

To effectively reduce the risk of developing blood clots, consider implementing the following preventive strategies:
By adopting these strategies, individuals can substantially lower their risk of developing blood clots while enhancing their overall cardiovascular health. Regular movement is emphasized by experts as a key factor in preventing DVT, with recommendations to incorporate activity into daily routines. Additionally, if you experience symptoms such as swelling, pain, or visible veins in your legs, it may indicate CVI or other vascular issues that require prompt attention. At Amavita Heart and Vascular Health, we offer comprehensive vascular assessments and treatments, including venous ablation, Varithena treatment, and sclerotherapy, to effectively address these concerns.

Understanding the treatment of blood clots in the leg is essential for effectively managing your health and preventing serious complications. By recognizing the symptoms, identifying risk factors, and exploring various treatment options, you can take proactive steps to safeguard your vascular health.
Key insights from this guide highlight the importance of early detection and intervention. Symptoms such as swelling, pain, and skin changes should not be overlooked, as they can lead to severe conditions like pulmonary embolism if not addressed promptly. The treatment landscape includes:
Each treatment is tailored to your specific needs. Furthermore, preventive strategies such as maintaining an active lifestyle and avoiding prolonged immobility are crucial in reducing the risk of clot formation.
Ultimately, awareness and education about blood clots can empower you to make informed decisions regarding your health. Engaging with healthcare providers about your personal risk factors and treatment options is vital. Taking these steps not only enhances your well-being but also contributes to broader public health efforts in combating the prevalence of blood clots. Prioritizing your vascular health today can lead to a healthier tomorrow.
What are blood clots and how do they form?
Blood clots, or thrombi, form when blood thickens and clumps together, often due to injury or prolonged immobility.
How does immobility contribute to blood clot formation?
Immobility, such as sitting for long periods during flights or resting in bed, can slow blood flow and significantly increase the risk of clot formation. Studies show that over one-third of venous thromboembolism (VTE) cases are linked to recent hospital stays.
What role does surgery play in the risk of blood clots?
Surgical procedures, especially those involving the legs or pelvis, can damage veins and raise the risk of clotting. VTE is a leading cause of preventable hospital death in the U.S., particularly after surgeries like total hip or knee joint replacements.
Which medical conditions increase susceptibility to blood clots?
Certain health issues, such as cancer and heart disease, can increase the risk of blood clots. Research indicates that up to 60% of cancer patients may die from clots rather than cancer itself.
How do hormonal factors influence blood clot risk?
Hormonal changes, such as those during pregnancy or from birth control pills, can increase the likelihood of clotting. Women are five times more likely to experience a VTE during pregnancy, childbirth, or in the three months following delivery.
What are the main risk factors for blood clots?
The main risk factors include age (over 60), obesity, smoking, a family history of blood clots, and a previous history of deep vein thrombosis (DVT) or pulmonary embolism (PE).
Can blood clots be prevented, and if so, how?
Yes, up to 70% of healthcare-associated VTE cases can be prevented through measures such as anticoagulant medications or compression stockings. Recognizing risk factors and taking preventive strategies are essential for managing health.