


Managing tachycardia can feel overwhelming, but understanding the condition is the first step toward better heart health. It’s important to recognize the different types of tachycardia and the symptoms that may arise. By exploring appropriate treatments, including medications and lifestyle adjustments, you can take proactive steps in your care journey.
Combining medical interventions, such as beta-blockers, with lifestyle changes—like stress management and dietary improvements—can make a significant difference. These strategies not only enhance heart health but also help mitigate the risks associated with tachycardia. Remember, you are not alone in this; many have found success in balancing medical care with supportive lifestyle choices.
If you have concerns about your heart health, consider reaching out to a healthcare professional. They can guide you through your options and provide the support you need. Taking these steps can lead to a healthier, more fulfilling life, filled with the peace of mind that comes from understanding your condition and taking charge of your health.
Understanding tachycardia is essential for anyone navigating the complexities of heart health. This condition, marked by an elevated heart rate, can manifest in various forms, each presenting its own unique challenges and risks. By exploring effective management strategies—such as medical treatments and lifestyle adjustments—you can empower yourself to take control of your heart health.
However, it's important to consider: what happens when the very medications meant to alleviate symptoms also introduce new concerns?
This article delves into vital steps for managing tachycardia, offering insights that could significantly enhance your well-being. Remember, you're not alone in this journey; support is available to help you every step of the way.
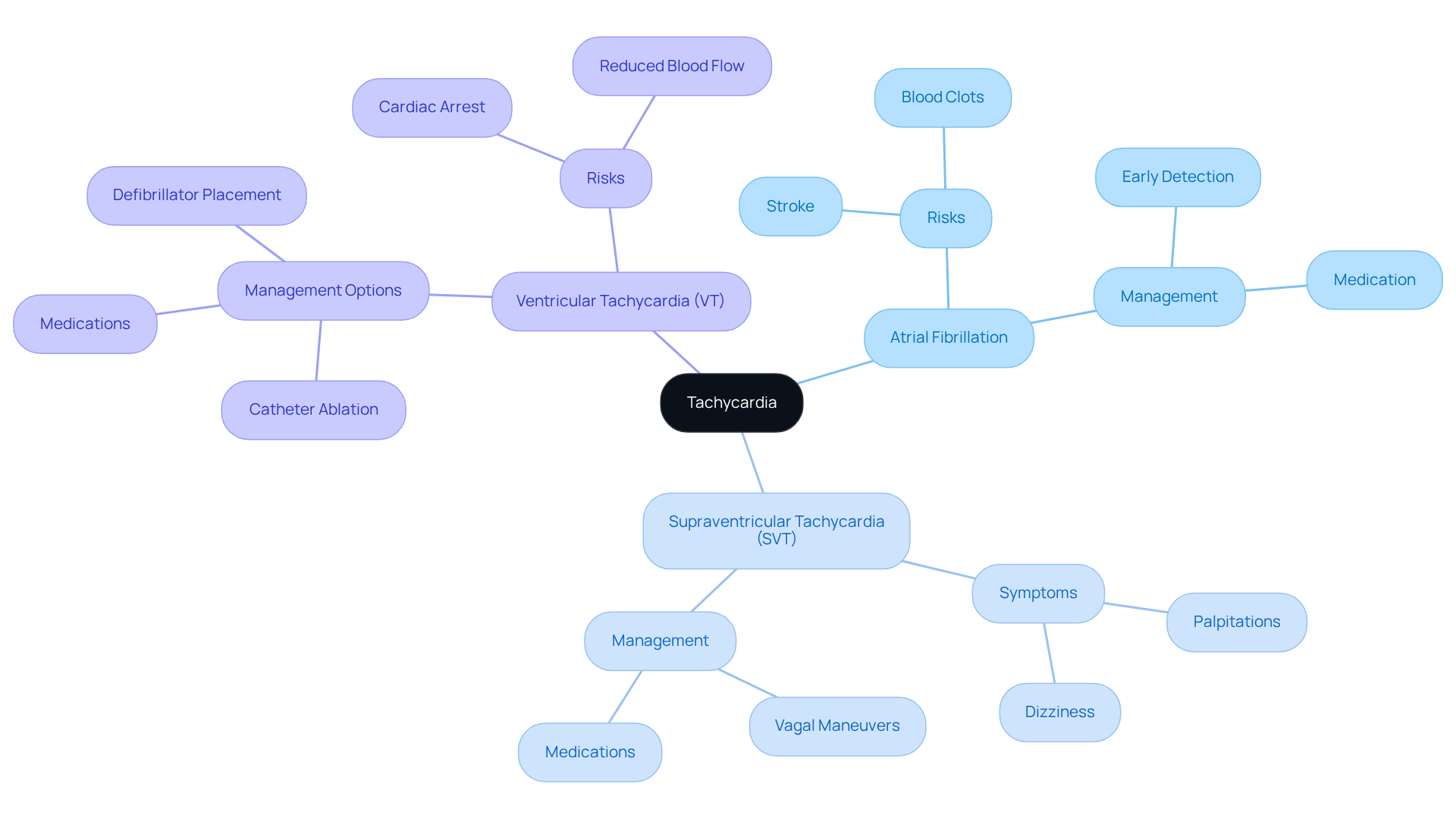
Tachycardia, a condition where the pulse rate exceeds the normal resting range—typically over 100 beats per minute—can understandably cause concern. It's important to know that this condition includes several types, each with unique implications for your health:
Understanding these forms of rapid heartbeat is essential for recognizing signs and pursuing prompt care. Unmanaged rapid heartbeat can lead to serious complications, such as heart failure and sudden cardiac death. If you or a loved one experiences any concerning symptoms, please reach out to a healthcare professional. Your health and well-being are our top priority, and we are here to .
Tachycardia can be concerning, and it's important to recognize its common symptoms, which include:
Understanding the causes of tachycardia can provide clarity and comfort. These causes may include:
Recognizing these symptoms and understanding their causes empowers you to take proactive steps in managing your condition. For instance, making lifestyle modifications such as reducing caffeine and alcohol intake, along with practicing stress management techniques, can help mitigate episodes. Furthermore, discussing your specific type of rapid heartbeat and possible treatment options with healthcare experts is essential for effective management. Remember, you are not alone in this journey, and there are supportive resources available to help you feel more at ease.

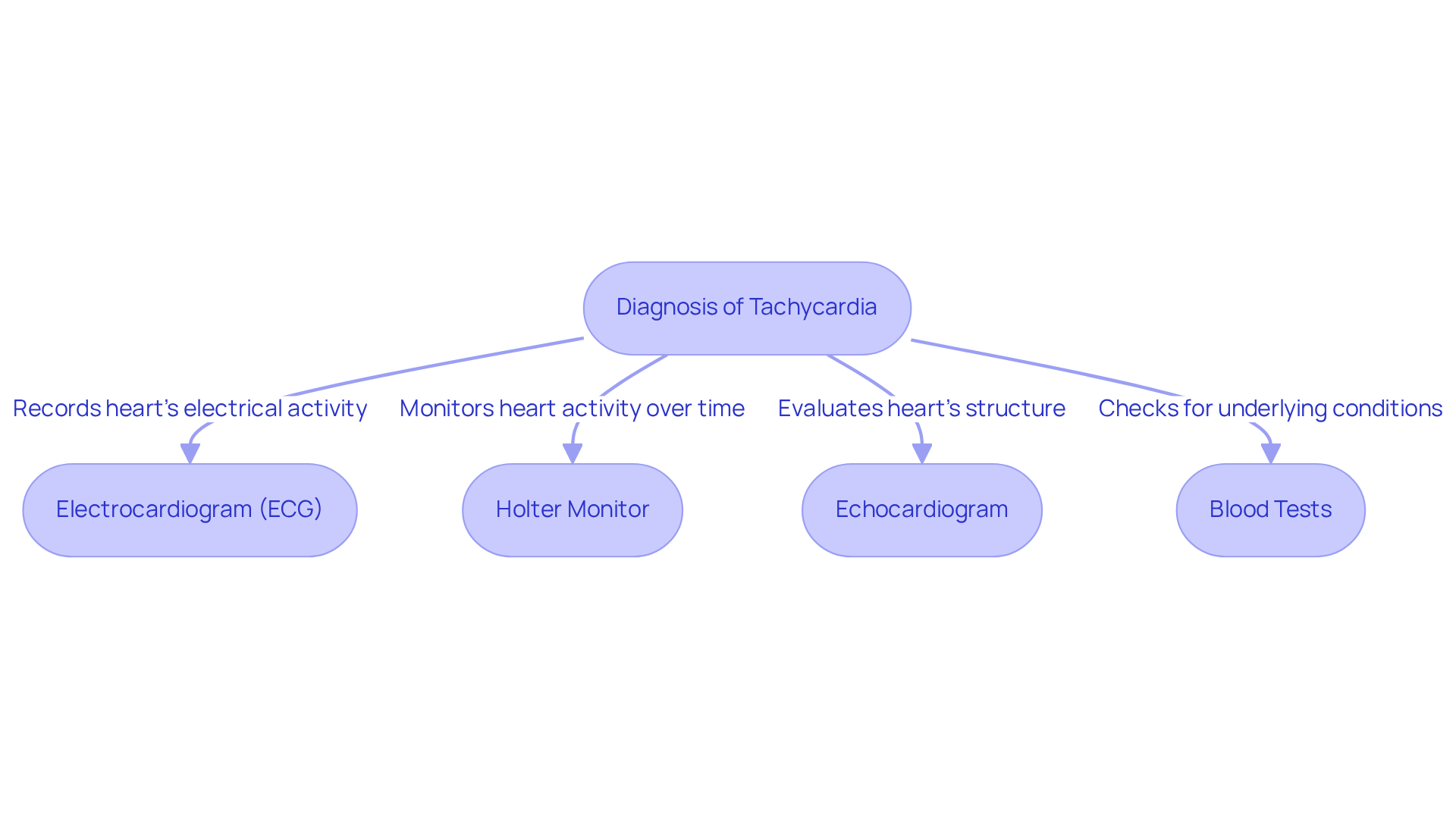
Diagnosing a rapid heart rate requires a comprehensive approach that emphasizes understanding your health concerns. This process includes reviewing your medical history, conducting physical examinations, and utilizing specific diagnostic tests. Here are some key tools that can help:
Recent advancements in ECG technology, including AI-enhanced algorithms, have significantly improved the accuracy of diagnosing tachycardia. These innovations enable earlier identification and better management of cardiovascular conditions, ultimately enhancing care for individuals like you. Understanding these diagnostic tools empowers you to , ensuring you feel supported every step of the way.
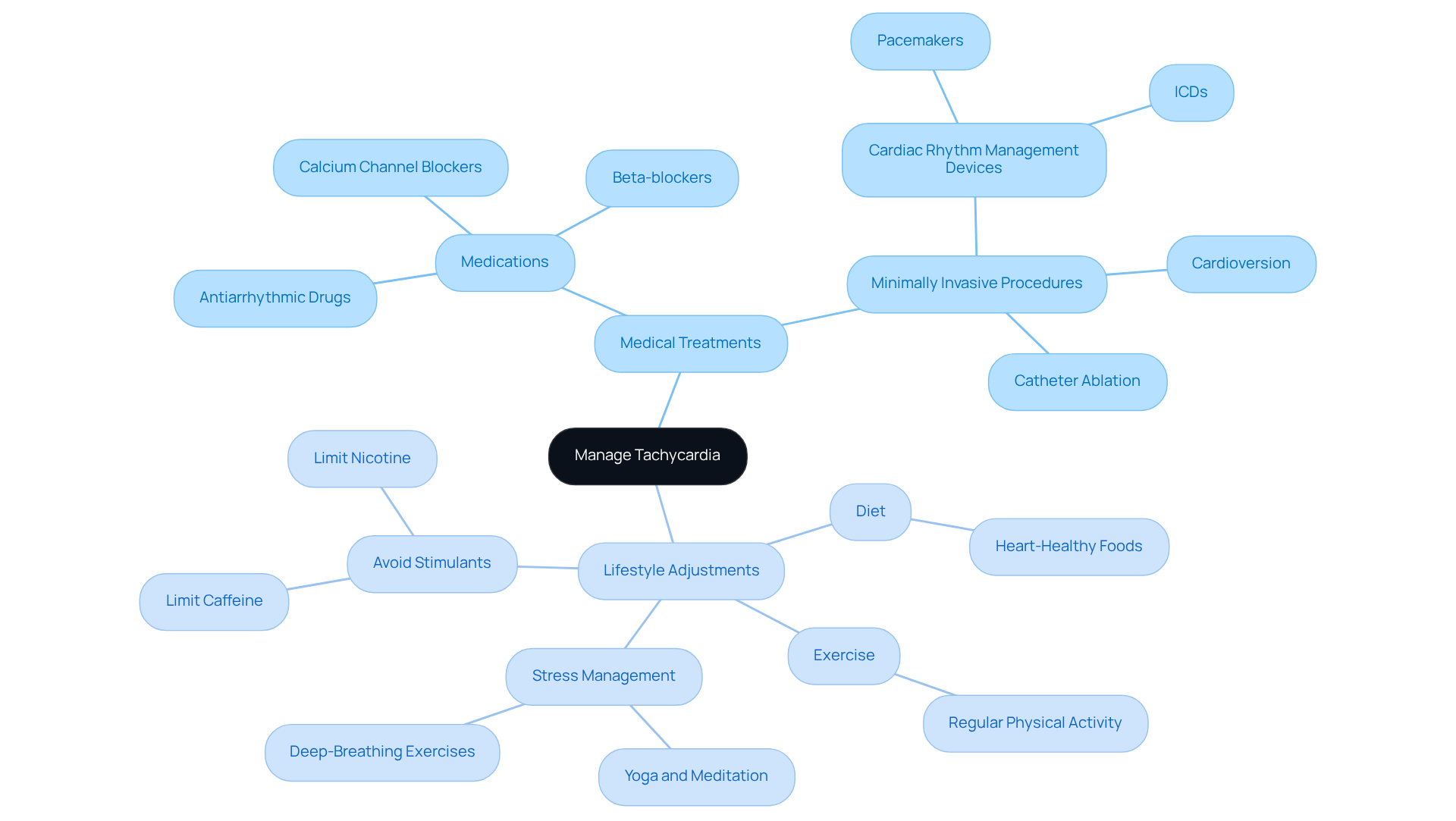
Managing tachycardia medicine effectively requires a comprehensive strategy that combines medical treatments with lifestyle modifications. It’s important to address your concerns and explore options that can truly make a difference in your heart health.
Medications: Beta-blockers, calcium channel blockers, and antiarrhythmic drugs are commonly prescribed to help regulate heart rate. These medications can significantly enhance symptoms and overall cardiac function. Beta-blockers, in particular, are especially effective in lowering pulse rate and preventing episodes of tachycardia medicine, providing you with relief and stability.
Minimally Invasive Procedures: For some individuals, catheter ablation may be a viable option. This procedure involves threading a catheter to the heart to create a scar that blocks abnormal electrical pathways, effectively . Many patients have found long-term success with catheter ablation, allowing them to reduce or eliminate their reliance on medications and regain control over their heart health.
Lifestyle Adjustments:
By integrating these treatment options and lifestyle changes, you can take proactive steps to manage your tachycardia. Remember, you are not alone on this journey; support is available, and together we can enhance your heart health and overall quality of life.
Understanding and managing tachycardia is essential for maintaining heart health and overall well-being. This guide outlines the crucial steps in recognizing, diagnosing, and treating this condition, emphasizing the importance of proactive engagement with healthcare providers. By being informed about the different types of tachycardia and their implications, you can take charge of your health and seek appropriate care when necessary.
Key insights include recognizing symptoms such as:
As well as understanding the various causes, ranging from heart-related issues to lifestyle factors. Diagnostic tools like ECGs and Holter monitors are vital for grasping the condition, while treatment options encompass:
Adopting a heart-healthy diet, engaging in regular exercise, and implementing effective stress management techniques can significantly enhance your heart health and reduce the risks associated with tachycardia.
Ultimately, managing tachycardia involves a blend of medical interventions and personal commitment to lifestyle changes. Encouraging you to actively participate in your healthcare journey not only empowers you but also fosters a supportive environment for better heart health. By taking these steps, you can lead a more fulfilling life, free from the limitations imposed by tachycardia. Remember, you are not alone in this journey, and support is always available.
What is tachycardia?
Tachycardia is a condition where the pulse rate exceeds the normal resting range, typically over 100 beats per minute.
What are the types of tachycardia?
The main types of tachycardia include Atrial Fibrillation, Supraventricular Tachycardia (SVT), and Ventricular Tachycardia (VT), each with different health implications.
What is Atrial Fibrillation and why is it concerning?
Atrial Fibrillation is an irregular and often rapid heart rate that can lead to serious complications such as blood clots, significantly increasing the risk of stroke. Early detection and management are crucial.
What symptoms might indicate Supraventricular Tachycardia (SVT)?
SVT is characterized by a rapid pulse and may lead to symptoms like palpitations and dizziness.
Do all individuals with SVT require treatment?
No, while many individuals with SVT may not require treatment, those experiencing frequent episodes could benefit from interventions like vagal maneuvers or medications.
What is Ventricular Tachycardia (VT) and why is it considered life-threatening?
Ventricular Tachycardia originates in the heart's lower chambers and can be life-threatening because it may lead to insufficient filling of the chambers, decreasing blood flow to the body.
How is Ventricular Tachycardia managed?
Management of VT often includes a combination of medications, catheter ablation, or the placement of a cardioverter defibrillator, especially in patients with underlying cardiac issues.
What are the potential complications of unmanaged tachycardia?
Unmanaged rapid heartbeat can lead to serious complications, including heart failure and sudden cardiac death.
What should I do if I experience concerning symptoms related to tachycardia?
If you or a loved one experiences concerning symptoms, it is important to reach out to a healthcare professional for prompt care.