


Understanding cardiovascular health can feel overwhelming, especially when it comes to choosing the right specialist. Many people wonder, "How do I know if I need a vascular doctor or a cardiologist?" Vascular doctors focus on issues related to blood vessels outside the heart, while cardiologists specialize in heart conditions. It’s crucial to distinguish between these two roles to ensure effective treatment.
This article explores the unique responsibilities and training of vascular doctors and cardiologists. By understanding their specific areas of expertise, you can make informed decisions about your health. Remember, it’s perfectly normal to feel uncertain when faced with symptoms that could fall under either category. You’re not alone in this journey.
If you’re experiencing symptoms that concern you, don’t hesitate to reach out for help. Consulting the right specialist can make all the difference in your care. Your health is important, and finding the right support is a vital step towards feeling better.
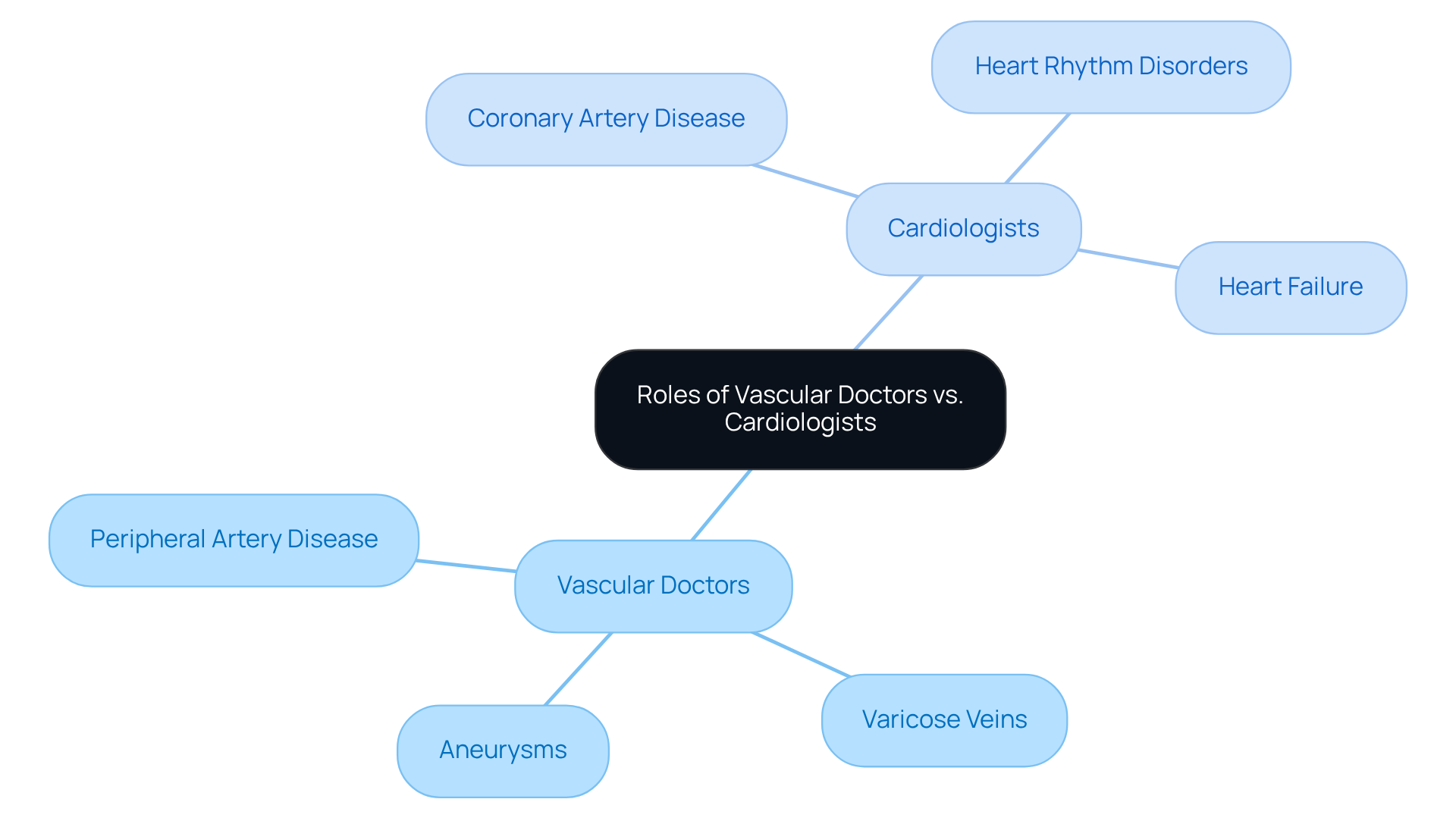
When it comes to your health, understanding the right specialists can make all the difference. Specialists in this field, often referred to as blood vessel doctors, are dedicated to diagnosing and treating issues related to blood vessels outside the heart and brain. They handle a variety of conditions, including:
On the other hand, cardiologists focus on the heart and its major blood vessels, managing conditions like:
Recognizing this distinction is crucial for you, as seeking the right specialist can significantly impact your treatment outcomes.
Unfortunately, many people are unaware of whether a vascular doctor is the same as a cardiologist and the differences between blood vessel specialists and cardiologists. This lack of understanding can lead to delays in receiving the appropriate care. For instance, if you're experiencing leg pain due to peripheral artery disease, you might mistakenly consult a cardiologist instead of a blood vessel specialist. This could prolong your discomfort and complicate your condition.
Healthcare professionals stress the importance of choosing the right specialist. One blood vessel specialist wisely noted, "Health care should be no different - select the top expert for the task." This highlights the need for you to be informed about your options. Blood vessel specialists are uniquely qualified to address circulatory disorders, employing both noninvasive and invasive treatments tailored to your individual needs. These may include:
Real-life examples show the positive outcomes linked to timely referrals to circulatory system specialists. Those who start treatment with a blood vessel specialist early often experience better long-term health results. For example, individuals treated for varicose veins by a blood vessel specialist frequently report significant relief from symptoms and an improved quality of life compared to those who delay seeking specialized care.
In conclusion, understanding if a vascular doctor is a vascular doctor the same as a cardiologist is essential for managing your cardiovascular health. By recognizing when to seek care from each specialist, you can make informed decisions that enhance your overall well-being. Remember, you are not alone in this journey; support is available, and taking the right steps can lead to a healthier, happier life.
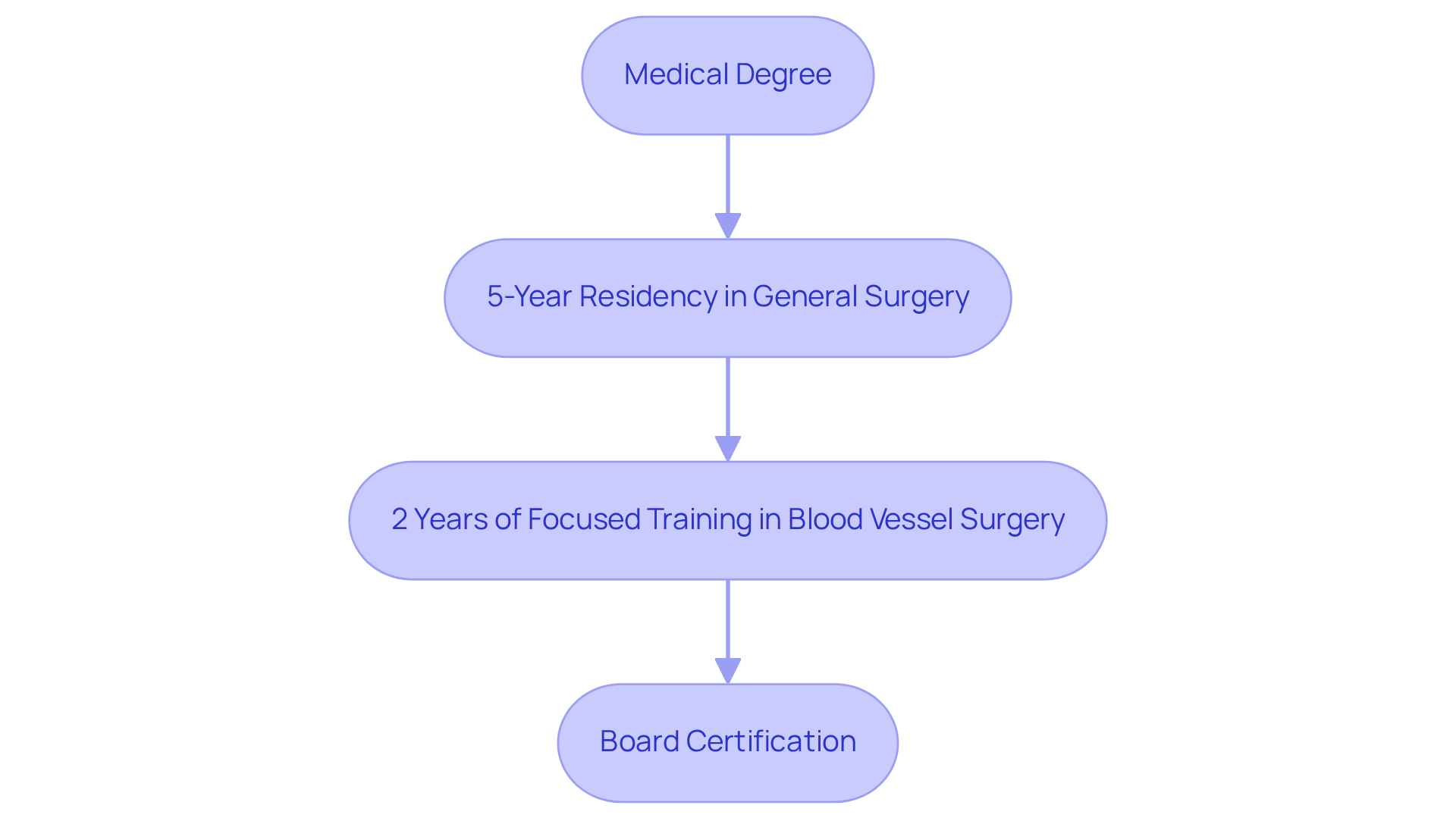
Becoming a specialist in blood vessels is a journey that begins with a medical degree, followed by a five-year residency in general surgery. After this foundational training, aspiring vascular surgeons typically undergo an additional two years of focused training in blood vessel surgery. Board certification in this specialty is crucial, as it ensures that the physician has met rigorous standards. This comprehensive training equips specialists with the skills needed to perform complex procedures and manage various circulatory conditions.
You might wonder why board certification matters. It’s widely recognized among healthcare practitioners as a mark of excellence. Not only does it confirm a doctor’s abilities, but it also enhances trust and safety for patients seeking care. Many specialists emphasize that board-certified blood vessel surgeons are more likely to achieve successful surgical outcomes due to their extensive training and commitment to high standards. Research shows that patients treated by board-certified vascular surgeons often experience lower complication rates and quicker recovery times compared to those cared for by non-certified surgeons.
In summary, the path to becoming a vascular physician is marked by thorough education and a dedication to excellence. This commitment ensures that patients receive the highest quality of care, allowing them to feel confident and supported throughout their treatment journey. If you have concerns about your vascular health, don’t hesitate to reach out for help. You deserve compassionate care and expert guidance.
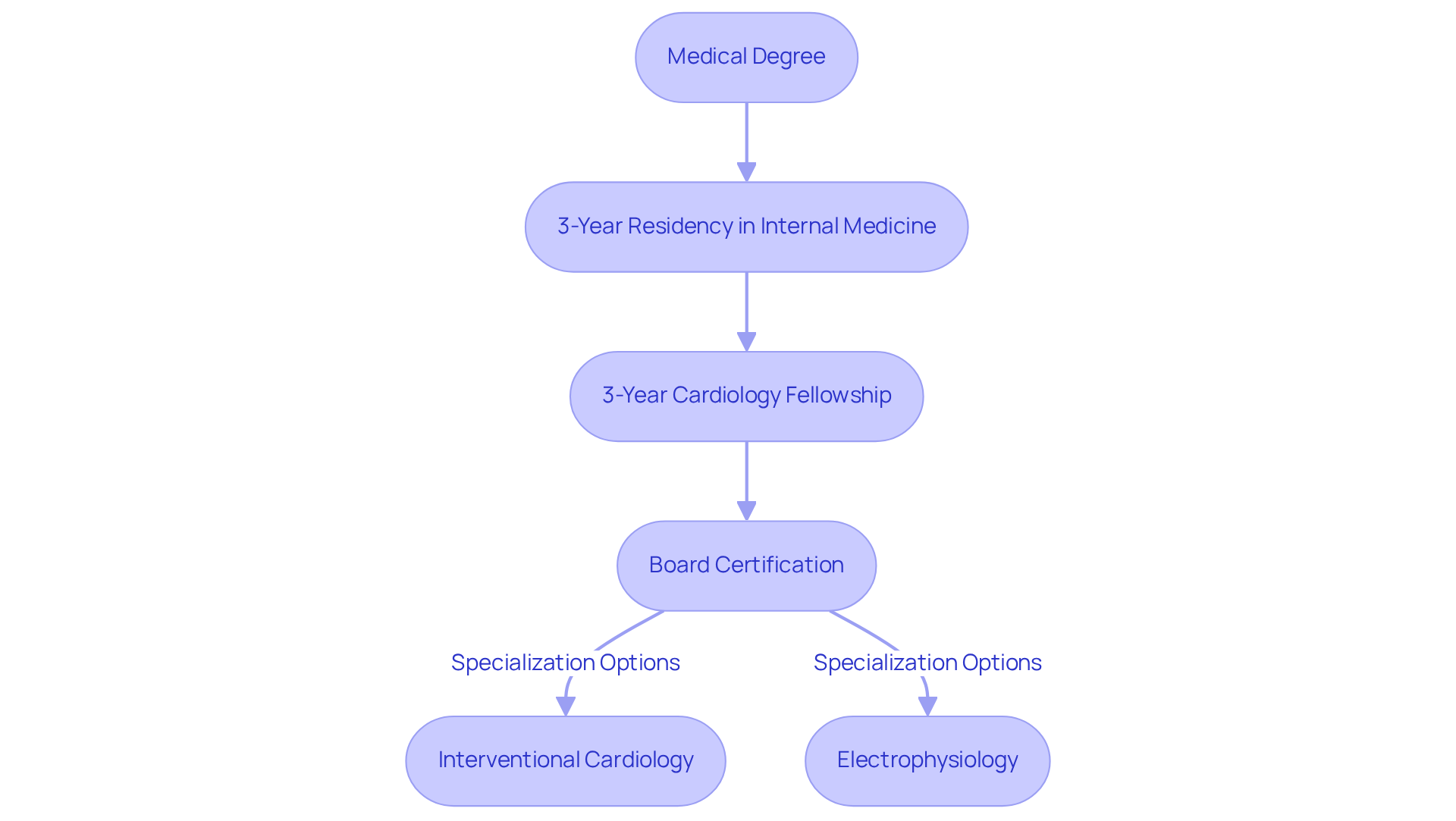
Becoming a cardiologist is a journey that begins with a medical degree, followed by a three-year residency in internal medicine. This foundational step is crucial for understanding the complexities of adult health. After completing residency, aspiring cardiologists enter a cardiology fellowship that lasts an additional three years. This fellowship provides comprehensive training in diagnosing and treating heart conditions, ultimately leading to better outcomes for patients.
Some cardiologists choose to further specialize in areas like interventional cardiology or electrophysiology, which requires additional training beyond the standard fellowship. Achieving board certification in cardiology is a significant milestone, as it shows that the physician has successfully passed rigorous examinations and is qualified to provide specialized heart care.
This extensive training, totaling a minimum of 14 years, equips cardiologists with the skills necessary to manage complex cardiovascular issues effectively. This ensures that patients receive the highest standard of care. At Amavita Heart and Vascular Health, we complement this expertise with advanced imaging capabilities and thorough assessments tailored for individuals at high risk, including those with diabetes, hypertension, or a family history of heart disease.
Furthermore, our CardioElite™ program enhances proactive management for patients, providing internal medicine doctors with advanced diagnostic data and 24/7 cardiology consultation. This approach not only improves outcomes but also helps reduce readmissions, ensuring that you feel supported every step of the way. If you have concerns about your heart health, don’t hesitate to reach out. We’re here to help you navigate your journey with compassion and care.
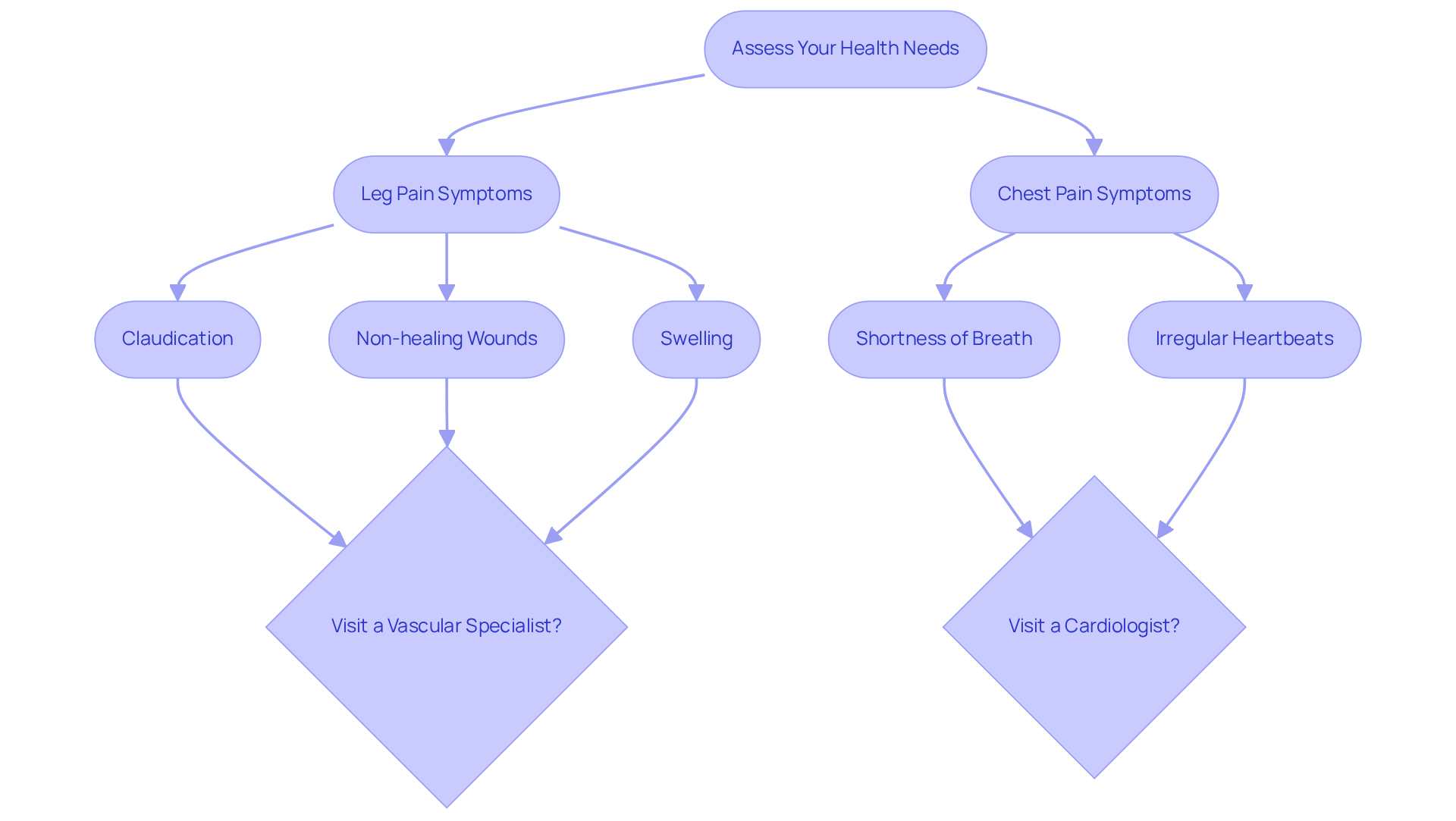
Begin by reflecting on your symptoms and health history. Are you experiencing leg pain during physical activity, known as claudication? Perhaps you have non-healing wounds or swelling in your legs? These key indicators may suggest it's time to visit a specialist, specifically, is a vascular doctor the same as a cardiologist? Conditions like Peripheral Artery Disease (PAD) and Chronic Venous Insufficiency (CVI) can lead to such symptoms, and addressing them promptly is crucial for your well-being.
Studies show that around 50% of individuals suffering from leg discomfort consult specialists in blood vessels. This statistic highlights the importance of seeking assistance without delay. Neglected circulatory issues can lead to severe complications, such as blood clots or even amputations. It's vital to obtain treatment to prevent these outcomes.
At Amavita Heart and Vascular Health, our specialists are here to support you. We utilize advanced diagnostic imaging to identify issues like PAD and CVI, ensuring comprehensive management tailored to your unique needs. We offer several minimally invasive treatments, including:
These options can provide relief with minimal downtime and no need for general anesthesia.
Conversely, if you encounter chest pain, shortness of breath, or irregular heartbeats, it raises the question of whether a vascular doctor is a vascular doctor the same as a cardiologist would be the more appropriate choice. Keeping a detailed record of your symptoms and any relevant medical history will facilitate a more productive consultation with your chosen specialist.
Remember, early detection and intervention can significantly improve health outcomes. It's crucial to seek help when these symptoms arise. You are not alone in this journey; we are here to help you every step of the way.
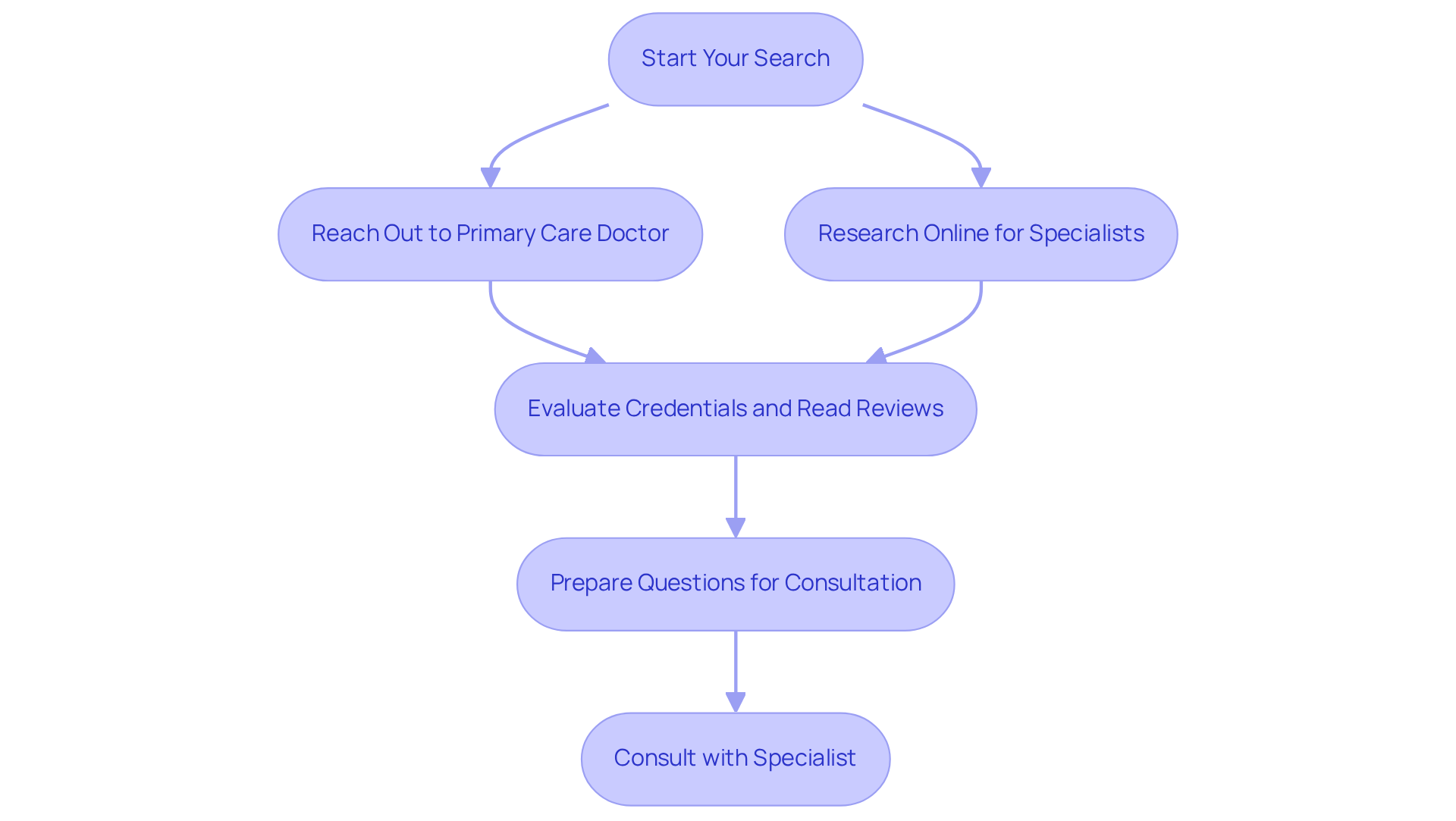
Finding the right blood vessel expert can feel overwhelming, but you don’t have to navigate this journey alone. Start by reaching out to your primary care doctor for a recommendation. Research shows that nearly 70% of individuals seek referrals for specialized treatment, and your doctor can guide you to trusted specialists.
Alternatively, consider searching online for board-certified vascular doctors or cardiologists in your area to find out if a vascular doctor is a vascular doctor the same as a cardiologist. Look for those who offer advanced imaging and comprehensive evaluations, like the dedicated team at Amavita Heart and Vascular Health. If you’re at high risk due to diabetes, hypertension, or a family history of heart disease, or if you’ve had inconclusive standard testing, Amavita’s services can be especially beneficial for you.
When evaluating potential specialists, take the time to verify their credentials and read client reviews. It’s important to ensure their experience aligns with your specific health concerns. As you prepare for your appointment, think about the questions you want to ask. For instance:
Preparing these questions will help you make the most of your consultation and empower you to make informed decisions about your vascular health.
At Amavita, specialists like Dr. Martinez-Clark integrate sophisticated tests into your comprehensive care plan. This level of cardiovascular care goes beyond what you might find at other practices, ensuring you receive the support you deserve. Remember, you’re not alone in this journey; there are compassionate professionals ready to help you every step of the way.
Understanding the differences between a vascular doctor and a cardiologist is vital for anyone looking to manage their cardiovascular health effectively. These specialists play distinct roles in the healthcare landscape. Vascular doctors focus on diagnosing and treating conditions related to blood vessels outside of the heart and brain, while cardiologists concentrate on heart-related issues. Recognizing these differences ensures that individuals receive the appropriate care they need, leading to better health outcomes.
Throughout this article, we've shared key insights about the specific conditions treated by each type of specialist, as well as the extensive training and qualifications required to practice in these fields. Vascular doctors are equipped to handle issues such as peripheral artery disease and varicose veins, utilizing both noninvasive and invasive treatments. In contrast, cardiologists are trained to address heart conditions like coronary artery disease and heart rhythm disorders. Understanding these nuances empowers you to seek the right care at the right time, ultimately enhancing your quality of life.
In a broader context, the significance of choosing the correct specialist cannot be overstated. Early detection and intervention can lead to improved health outcomes and prevent severe complications. Whether you're seeking a vascular doctor for circulatory issues or a cardiologist for heart-related symptoms, being proactive in your health management is crucial. By making informed decisions and consulting the right experts, you can navigate your health journey with confidence, ensuring you receive the compassionate care and expert guidance you deserve.
What is the difference between vascular doctors and cardiologists?
Vascular doctors, also known as blood vessel specialists, focus on diagnosing and treating issues related to blood vessels outside the heart and brain, such as peripheral artery disease, varicose veins, and aneurysms. Cardiologists, on the other hand, specialize in the heart and its major blood vessels, managing conditions like coronary artery disease, heart rhythm disorders, and heart failure.
Why is it important to understand the roles of vascular doctors and cardiologists?
Understanding the distinct roles of these specialists is crucial for seeking appropriate care and treatment. Consulting the wrong specialist can delay diagnosis and treatment, potentially worsening health conditions.
What types of treatments do vascular doctors provide?
Vascular doctors offer both noninvasive and invasive treatments tailored to individual needs. Common procedures include venous ablation, Varithena therapy, and sclerotherapy for conditions like Chronic Venous Insufficiency (CVI).
What qualifications and training do vascular doctors have?
Vascular doctors typically complete a medical degree, followed by a five-year residency in general surgery, and an additional two years of focused training in blood vessel surgery. Board certification in this specialty is essential, confirming that the physician has met rigorous standards.
Why is board certification important for vascular doctors?
Board certification is recognized as a mark of excellence among healthcare practitioners. It ensures that a doctor has the necessary skills and training, which can lead to better surgical outcomes, lower complication rates, and quicker recovery times for patients.
How can seeing a vascular doctor early impact health outcomes?
Patients who seek care from a vascular specialist early often experience better long-term health results. For instance, individuals treated for varicose veins by a vascular doctor frequently report significant relief from symptoms and an improved quality of life compared to those who delay seeking specialized care.