


Understanding the complexities of heart failure is vital, especially for those navigating the challenging realities of its final stages. End-stage heart failure brings debilitating symptoms and significant lifestyle changes, making it essential to focus on informed care strategies.
How can caregivers and healthcare providers effectively recognize and manage these critical symptoms to enhance the quality of life for patients?
This article explores the symptoms, treatment options, and compassionate care strategies that are crucial for individuals facing advanced cardiac dysfunction.
End-stage cardiac dysfunction, often referred to as advanced cardiac insufficiency, represents the final stages of heart failure. At this stage, the heart's ability to pump blood is significantly diminished, leading to persistent and debilitating symptoms that can deeply affect daily life. Patients may experience:
Recognizing these symptoms is vital for caregivers and healthcare providers, as it highlights the urgent need for appropriate care and interventions.
At Amavita Heart and Vascular Health®, we understand how overwhelming this can be. That’s why we prioritize comprehensive cardiac evaluations and preventive strategies to help manage these symptoms effectively. Our approach to preventive cardiology combines advanced risk assessment tools with personalized interventions, addressing key risk factors like:
Did you know that around 6.7 million Americans are currently living with heart failure? A significant number of these individuals are diagnosed with the final stages of heart failure, highlighting the urgent need for effective management strategies.
Research shows that innovative therapies, such as left-ventricular assist devices (LVADs) paired with advanced pharmacological treatments, can lead to remarkable recovery in certain patients. In a recent study, 11 out of 15 individuals experienced significant improvement, allowing them to have their LVADs removed and return to active lives post-treatment. This offers hope, showing that some aspects of final stages of heart failure can be reversed, potentially easing the burden on transplant waiting lists.
Our cardiologists at Amavita emphasize the importance of recognizing the signs of advanced cardiac dysfunction. This includes not just the physical symptoms but also the psychological and social challenges that patients face. Addressing these multifaceted needs is essential for improving outcomes and enhancing quality of life. Moreover, it’s crucial to acknowledge that racial disparities exist in cardiac hospitalization rates, particularly among Black patients, highlighting the need for targeted interventions. As the incidence of cardiac dysfunction rises, especially among older adults and underserved communities, understanding and managing these advanced cardiac issues becomes increasingly important in cardiovascular care. The economic impact is significant too, with estimates suggesting that direct medical costs will reach $53 billion by 2030, further emphasizing the need for effective management strategies.

Common symptoms of the final stages of heart failure can be quite distressing, and recognizing them is crucial for providing the right support. Here are some key signs to watch for:
Severe shortness of breath (dyspnea): Many patients find it challenging to breathe, even when resting. This can be very uncomfortable, and it’s important to manage this symptom carefully.
Ongoing coughing or wheezing: This often happens due to fluid buildup in the lungs, indicating that the heart isn’t functioning as well as it should.
Fatigue and weakness: A significant drop in energy can make even the simplest tasks feel overwhelming. This highlights the importance of having extra support during this time.
Swelling (edema): Fluid retention may occur in the legs, abdomen, and other areas, which can signal that the heart is struggling to pump blood effectively, particularly in the final stages of heart failure.
Reduced appetite and weight reduction: Many individuals may lose interest in food, leading to weight loss that can complicate their health further.
Understanding these symptoms is essential for caregivers. It empowers them to provide the necessary support and seek timely medical assistance when needed. Remember, you’re not alone in this journey; reaching out for help can make a significant difference.

When facing the final stages of heart failure, it's natural to have concerns about your health and quality of life. There are various treatment alternatives available that focus on enhancing outcomes and providing compassionate care. Medications play a vital role in this journey. Diuretics can help relieve fluid buildup, while ACE inhibitors and beta-blockers work to improve heart function. Recently, sodium-glucose cotransporter-2 (SGLT2) inhibitors have emerged, showing significant benefits for individuals with cardiac dysfunction, especially those with preserved ejection fraction (HFpEF).
Device therapy is another important option, particularly for those who may not be candidates for transplantation. Implantable cardioverter-defibrillators (ICDs) and left ventricular assist devices (LVADs) have proven effective in managing symptoms of advanced cardiac failure. Studies have shown that LVADs can significantly enhance survival rates and improve quality of life, serving as a bridge to transplantation or as a long-term solution for those who cannot undergo surgery.
Heart transplantation remains a transformative choice for eligible individuals, offering the potential for substantial improvements in both quality of life and longevity. However, the limited availability of donor hearts makes it crucial to explore all possible therapies.
Palliative support is equally important, focusing on symptom management and enhancing the overall quality of life for individuals in the final stages of heart failure. This comprehensive approach ensures that patients receive compassionate support tailored to their unique needs, empowering caregivers to advocate effectively for their loved ones.
In addition to these traditional treatment options, Amavita's CardioElite™ program stands out as a valuable resource, providing a holistic approach to cardiovascular management in skilled nursing facilities (SNFs). By offering advanced, real-time diagnostic information and 24/7 cardiology consultation, CardioElite™ enhances proactive management and addresses the high rates of cardiovascular readmissions often seen in SNFs. This program combines AI with AHA certification, ensuring that patients receive personalized, data-driven support.
Understanding these treatment options, including the innovative assistance offered by Amavita's CardioElite™ program, empowers families to make informed decisions during challenging times. Remember, you are not alone in this journey, and there are compassionate resources available to help you navigate through advanced cardiac deterioration.

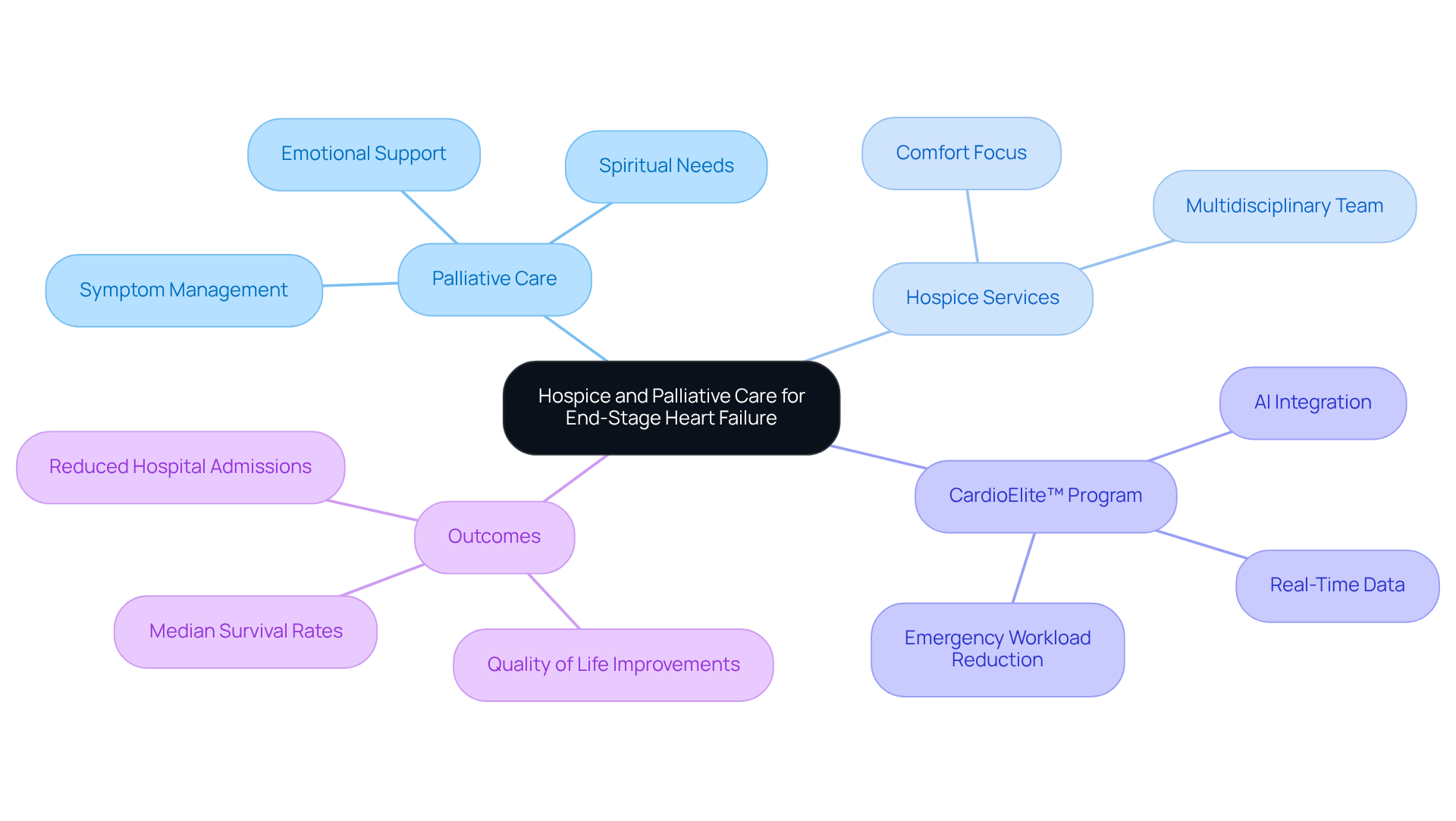
Hospice and palliative support play a vital role in managing the final stages of heart failure, significantly enhancing the quality of life for individuals. Palliative care aims to ease symptoms and improve overall well-being at any stage of the illness, providing essential support to both individuals and their families. This compassionate approach focuses on comprehensive symptom management, addressing physical discomfort, emotional distress, and spiritual needs, which becomes increasingly important as heart failure progresses.
In addition to this, Amavita's CardioElite™ program complements these efforts by offering advanced, real-time diagnostic data and 24/7 cardiology consultation. This proactive management enhances the care individuals receive. By integrating technology, including AI and AHA certification, the program not only supports symptom management but also helps reduce the emergency workload for healthcare providers. This is particularly important in addressing the high cardiovascular readmission rates often seen in skilled nursing facilities (SNFs). The CardioElite™ program acts as a clinical force multiplier, empowering SNFs to manage cardiac individuals more effectively.
On the other hand, hospice services are tailored for individuals with a prognosis of six months or less, focusing on comfort and support rather than curative treatments. It provides a compassionate environment where individuals can receive care that honors their dignity and choices. Both hospice and palliative support involve a dedicated multidisciplinary team committed to ensuring that individuals experience a holistic approach to their treatment during this challenging time.
Real-life examples highlight the effectiveness of palliative support in cardiac management. Studies indicate that 39% of individuals with cardiac issues receiving supportive treatment reported significant improvements in their condition after six months, with quality of life scores increasing by approximately 12.92 points. Furthermore, individuals in hospice support experienced fewer emergency department visits and hospital admissions, leading to a median survival of 80 days compared to 71 days for those who did not enroll.
Experts emphasize the importance of symptom control in cardiac insufficiency. A personalized strategy for palliative support can greatly enhance individual satisfaction and emotional wellness, ultimately resulting in better health outcomes. Understanding the difference between hospice and palliative care is crucial for individuals and families navigating the complexities of heart failure, particularly in the final stages of heart failure, to ensure they receive the most appropriate support at each stage of the illness. Amavita's CardioElite™ program represents a meaningful opportunity to improve cardiac services and outcomes, further supporting patients and families during this critical time.
End-stage heart failure marks a crucial point in the journey of cardiac health, where the heart struggles to function effectively. Recognizing this stage is vital for both patients and caregivers, as it calls for immediate and specialized care to alleviate distressing symptoms and improve quality of life.
Have you noticed signs like extreme fatigue, shortness of breath, or fluid retention? These symptoms are key indicators of advanced heart failure. Exploring treatment options, including innovative therapies like LVADs and comprehensive palliative care, highlights the importance of a holistic approach to managing this condition. Programs like Amavita's CardioElite™ show how technology and personalized care can truly make a difference in patient outcomes during these challenging times.
Understanding the final stages of heart failure and the care options available is essential for patients and their families. This knowledge empowers individuals to seek the support they need and underscores the significance of compassionate care in enhancing life quality. As awareness grows around the complexities of heart failure, it’s crucial for healthcare providers and communities to unite in ensuring that those affected receive the comprehensive care they deserve.
Remember, you’re not alone in this journey. Reach out for support, and let’s work together to navigate these difficult times with understanding and compassion.
What is end-stage heart failure?
End-stage heart failure, also known as advanced cardiac insufficiency, is the final stage of heart failure where the heart's ability to pump blood is severely diminished, leading to persistent symptoms that significantly affect daily life.
What symptoms are associated with end-stage heart failure?
Patients may experience extreme fatigue, shortness of breath even while resting, and noticeable fluid retention that can cause swelling in the legs and abdomen.
Why is it important to recognize the symptoms of end-stage heart failure?
Recognizing these symptoms is vital for caregivers and healthcare providers as it highlights the urgent need for appropriate care and interventions.
How does Amavita Heart and Vascular Health® approach the management of end-stage heart failure?
Amavita prioritizes comprehensive cardiac evaluations and preventive strategies, combining advanced risk assessment tools with personalized interventions to manage symptoms effectively.
What are some key risk factors addressed in the preventive cardiology approach?
Key risk factors include family history, high blood pressure, high cholesterol, and diabetes.
How many Americans are currently living with heart failure?
Approximately 6.7 million Americans are living with heart failure, with a significant number diagnosed at the final stages.
What innovative therapies are available for patients with end-stage heart failure?
Innovative therapies such as left-ventricular assist devices (LVADs) combined with advanced pharmacological treatments can lead to remarkable recovery in certain patients.
What does recent research indicate about the effectiveness of LVADs?
Recent studies show that 11 out of 15 individuals experienced significant improvement after treatment with LVADs, allowing them to have the devices removed and return to active lives.
What additional challenges do patients with advanced cardiac dysfunction face?
Patients face not only physical symptoms but also psychological and social challenges, which are essential to address for improving outcomes and quality of life.
Are there disparities in cardiac hospitalization rates?
Yes, racial disparities exist in cardiac hospitalization rates, particularly among Black patients, highlighting the need for targeted interventions.
What is the projected economic impact of cardiac dysfunction by 2030?
Direct medical costs related to cardiac dysfunction are estimated to reach $53 billion by 2030, emphasizing the need for effective management strategies.