


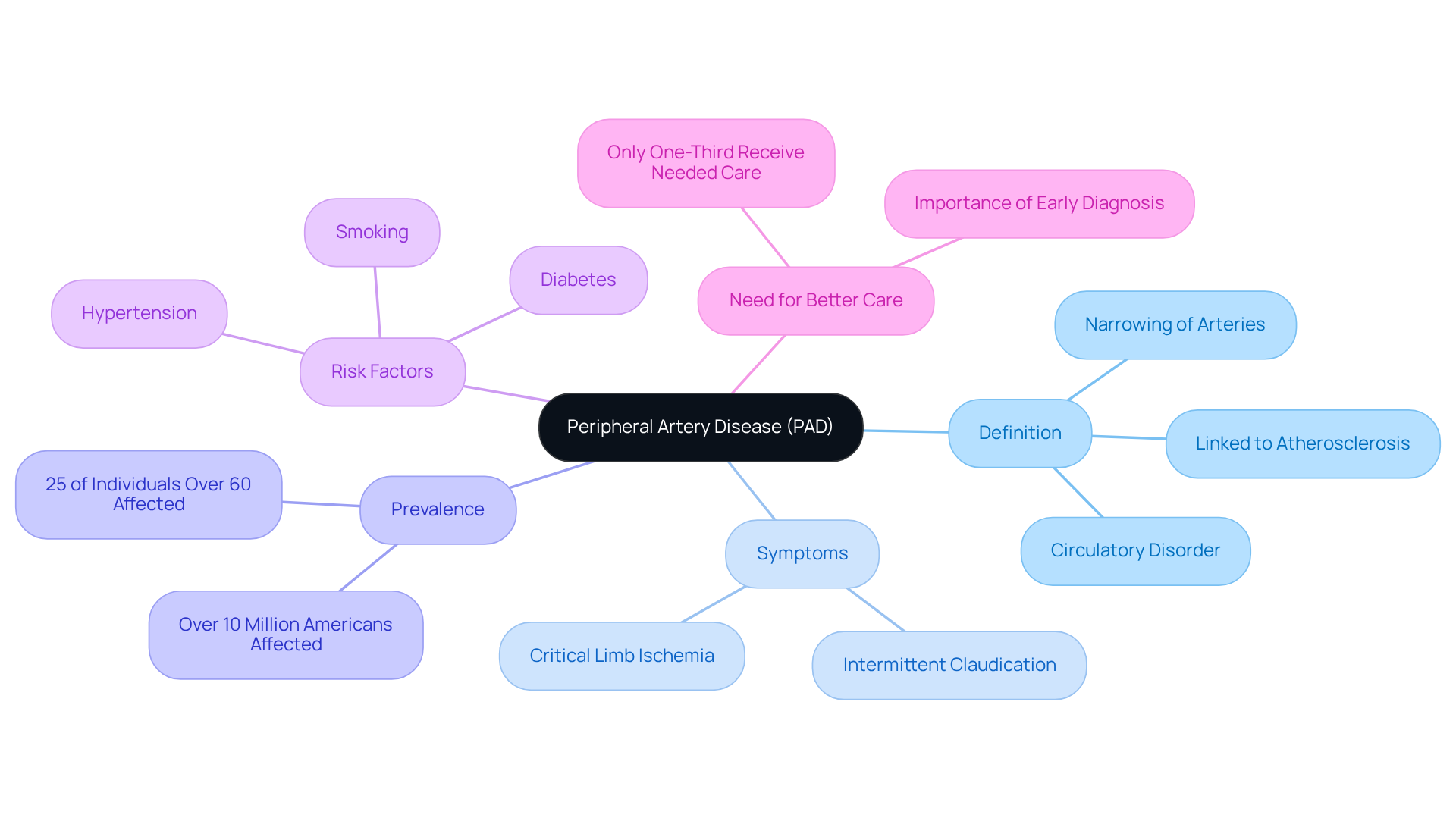
Peripheral Artery Disease (PAD) is a common yet often overlooked circulatory disorder that can significantly impact seniors, affecting their mobility and overall quality of life. Did you know that as many as 25% of individuals over 60 experience this condition? It can lead to debilitating pain and increase the risk of serious complications.
Understanding the nuances of PAD - from its risk factors and symptoms to the diagnostic procedures and treatment options available - can empower seniors and their caregivers. By taking proactive steps toward better vascular health, you can enhance your well-being.
How can one navigate the complexities of PAD diagnosis and management? It’s essential to know that you’re not alone in this journey. With the right support and information, you can work towards a healthier, more independent life. Remember, reaching out for help is a sign of strength, and there are resources available to guide you.
Peripheral Artery Disease (PAD) is a common circulatory disorder that affects many, particularly as we age. It occurs when arteries narrow, restricting blood flow to the limbs, especially the legs. This condition is often linked to atherosclerosis, where fatty deposits build up in the arterial walls. For those over 60, about 25% are impacted by PAD, leading to discomfort such as leg pain or cramping during physical activities. This can significantly limit mobility and affect daily life. Have you or someone you know experienced difficulty walking even short distances? It’s a challenge that can impact independence and routine activities.
Sadly, recent studies show that only about one-third of individuals receive the care they truly need. This highlights a pressing need for better screening and treatment options. Key signs of PAD include:
Current research continues to explore the underlying causes of PAD, revealing that factors like diabetes, smoking, and hypertension can significantly increase risk. Addressing these concerns through early diagnosis and intervention is vital. By taking proactive steps, we can enhance patient outcomes and improve quality of life. Remember, you’re not alone in this journey. Seeking help and support can make a world of difference.
Peripheral artery disease diagnosis can be a concerning issue, especially for older adults. Understanding the factors that contribute to its development is crucial for taking charge of your health. Here are some key factors to consider:
Research shows that smoking is particularly harmful, especially for seniors. Studies indicate that quitting smoking can significantly lower your risk of PAD. By understanding these risk factors, you can take proactive steps to manage your cardiovascular health and improve the likelihood of a peripheral artery disease diagnosis. Remember, you’re not alone in this journey. Seeking support and making lifestyle changes can lead to better outcomes and reduce the need for invasive procedures. Your health matters, and taking these steps can help you lead a healthier, more fulfilling life.

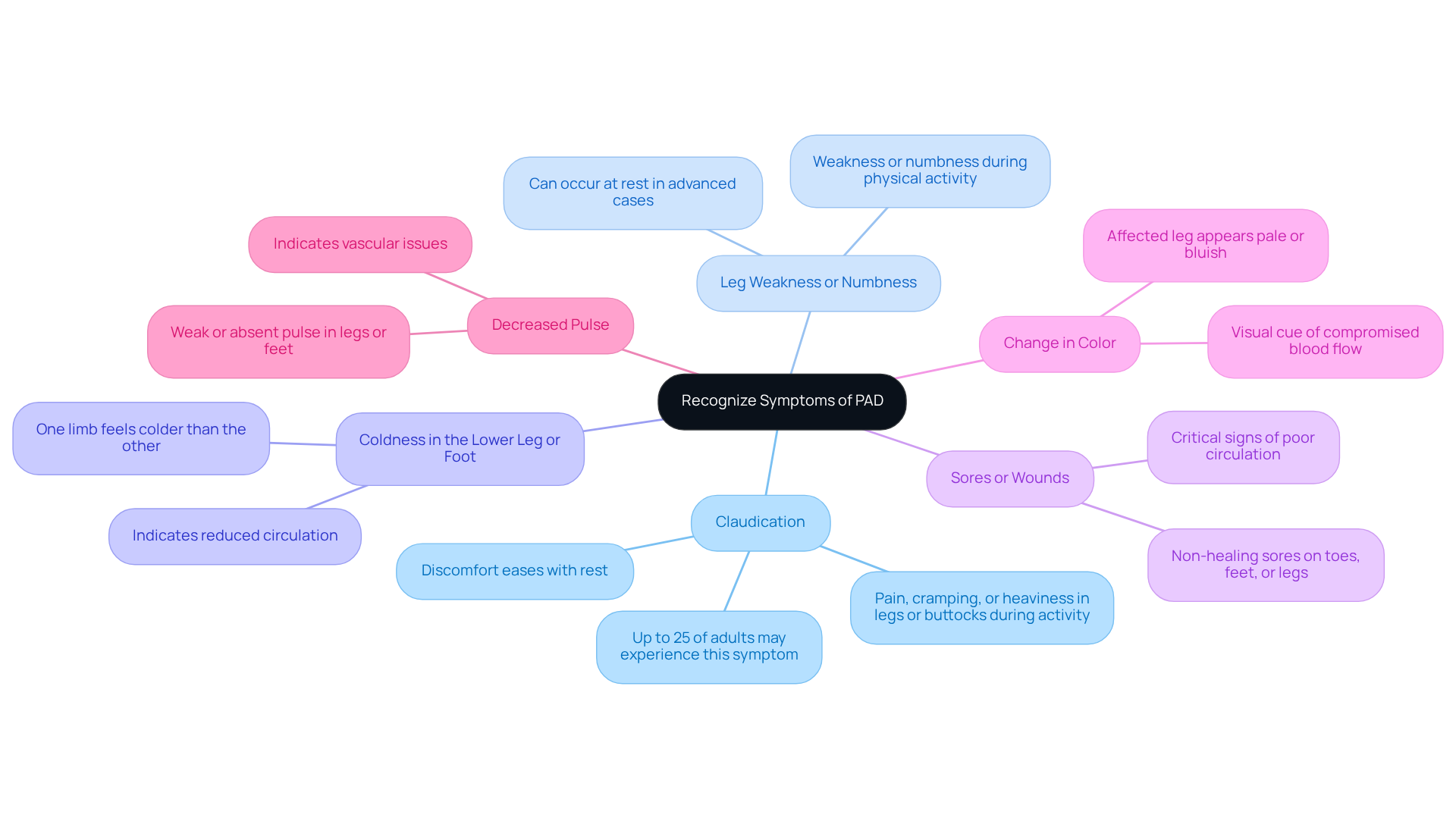
Recognizing the symptoms for a peripheral artery disease diagnosis is crucial, especially for seniors who may experience unique manifestations of the condition. If you or a loved one is at high risk-perhaps due to diabetes, hypertension, or a family history of heart disease-it's essential to be vigilant. Here are some common indicators to watch for:
Claudication: This symptom often presents as pain, cramping, or heaviness in the legs or buttocks during activities like walking or climbing stairs. The good news is that this discomfort usually eases with rest. Research shows that up to 25% of adults may experience claudication, and its prevalence increases significantly in those over 50.
Leg Weakness or Numbness: You might notice weakness or numbness in your legs during physical activity. In more advanced cases of PAD, this sensation can even occur at rest.
Coldness in the Lower Leg or Foot: If one limb feels noticeably colder than the other, it could indicate reduced circulation, which is a sign to pay attention to.
Sores or Wounds: Non-healing sores or wounds on the toes, feet, or legs are critical signs of poor circulation and should prompt immediate medical attention.
Change in Color: If the affected leg appears pale or bluish, it’s a visual cue that blood flow is compromised.
Decreased Pulse: During a physical examination, a weak or absent pulse in the legs or feet can be detected, further indicating vascular issues.
At Amavita Heart and Vascular Health, our vascular specialists emphasize the importance of recognizing these symptoms early for an accurate peripheral artery disease diagnosis. One expert notes, 'Getting a peripheral artery disease diagnosis early can prevent serious complications,' highlighting the importance of proactive health management. It’s common for many seniors to dismiss leg pain as just a normal part of aging, but this can lead to severe consequences if PAD is left untreated. Factors like smoking, diabetes, and age significantly heighten the likelihood of developing PAD, making awareness even more crucial.
By understanding these symptoms and their implications, you can advocate for your health and seek timely intervention, ultimately improving your quality of life. Amavita's advanced imaging capabilities, including minimally invasive procedures, ensure that individuals at high risk receive comprehensive evaluations and targeted cardiovascular care tailored to their needs.
Diagnosing peripheral artery disease diagnosis can feel overwhelming, but understanding the process can help ease your concerns. Here’s a gentle overview of the key steps involved:
At Amavita Heart and Vascular Health, Dr. Martinez-Clark’s Harvard training and extensive cardiovascular experience ensure that these sophisticated tests are seamlessly integrated into your care plan. Recent advancements in the diagnosis of peripheral artery disease, particularly the ABI test, have shown significant promise in early detection. Studies indicate that systematic screening can transform reactive care into cost-effective preventive management, ultimately reducing the risk of serious complications like foot ulcers and amputations.
It’s concerning to note that 29% of individuals with diabetes mellitus remain undiagnosed for PAD. This condition often goes unnoticed, especially in older adults, making proactive screening crucial for improving outcomes and enhancing quality of life. As experts emphasize, early detection through systematic screening provides a path forward for peripheral artery disease diagnosis, transforming expensive reactive care into cost-effective preventive management.
If you have any concerns about your vascular health, please don’t hesitate to reach out. We’re here to support you every step of the way.

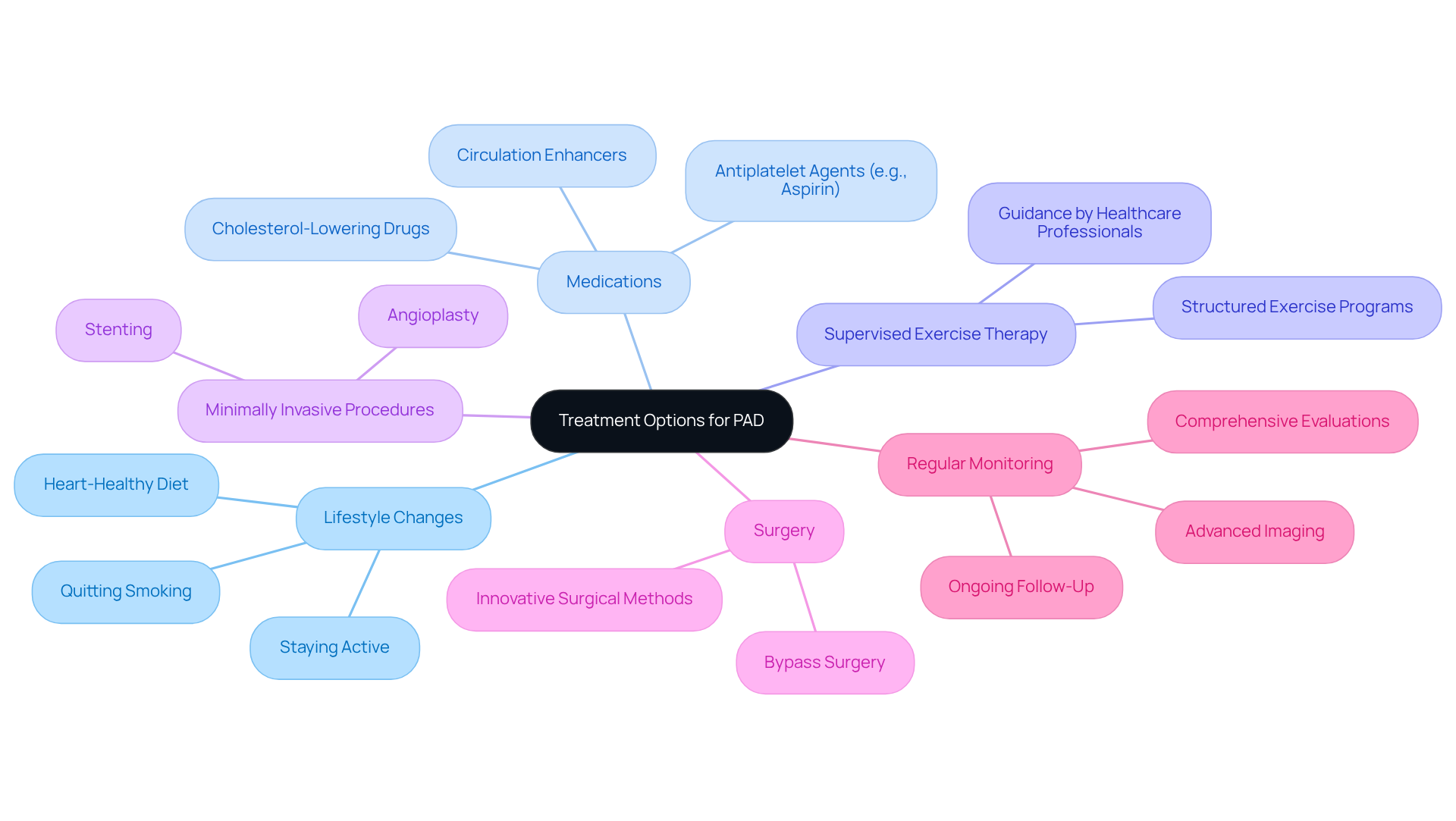
At Amavita Heart and Vascular Health, we understand that living with a peripheral artery disease diagnosis can be challenging. Our treatment approach focuses on improving your symptoms and preventing complications, all while putting you at the center of your care. Here’s how we can help:
Moreover, Amavita Research Services plays a vital role in advancing cardiovascular care. We ensure that our treatment options are informed by the latest research findings, benefiting individuals at high risk, including those with diabetes, hypertension, or a family history of heart disease.
At Amavita, we are committed to providing innovative cardiovascular care that is personalized for you. We understand that each patient has unique needs, and we strive to enhance your quality of life through our compassionate approach. If you have any concerns or questions, please don’t hesitate to reach out. We’re here to support you every step of the way.
Understanding Peripheral Artery Disease (PAD) is crucial for seniors, as early diagnosis and intervention can greatly enhance quality of life. This article highlights the importance of recognizing symptoms, understanding risk factors, and exploring the diagnostic and treatment options available for those affected by this condition. By being informed, individuals can take meaningful steps towards managing their health and preventing complications associated with PAD.
Key insights include the prevalence of PAD among seniors, especially those over 60, and the critical symptoms such as claudication and leg weakness that should not be overlooked. It’s essential to pay attention to these signs. The article also emphasizes the role of lifestyle modifications, medications, and advanced treatment options, including minimally invasive procedures, in managing PAD effectively. Furthermore, the significance of regular monitoring and comprehensive evaluations cannot be understated, as they are vital for tailoring care to individual needs.
As awareness of Peripheral Artery Disease grows, it’s important for seniors and their caregivers to prioritize cardiovascular health. Engaging in preventive measures, seeking timely medical advice, and advocating for regular screenings can lead to better health outcomes. Have you considered how understanding PAD and its implications can empower you? By taking these steps, individuals can lead healthier, more fulfilling lives, ultimately enhancing their independence and well-being. Remember, you’re not alone in this journey; support is available, and taking action today can make a difference.
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease (PAD) is a common circulatory disorder that occurs when arteries narrow, restricting blood flow to the limbs, particularly the legs. It is often linked to atherosclerosis, where fatty deposits build up in the arterial walls, and affects about 25% of individuals over 60.
What are the symptoms of PAD?
Key symptoms of PAD include intermittent claudication, which is pain during physical exertion that eases with rest, and critical limb ischemia, which can lead to serious complications such as amputation.
What are the risk factors for developing PAD?
The main risk factors for developing PAD include age (especially over 50), smoking, diabetes, high blood pressure, high cholesterol, family history of heart disease or PAD, and a sedentary lifestyle.
How does smoking affect the risk of PAD?
Smoking is the most significant adjustable risk factor for PAD, as it damages blood vessels and accelerates atherosclerosis, greatly increasing the chances of developing the condition. Quitting smoking can significantly lower this risk.
Why is early diagnosis and intervention important for PAD?
Early diagnosis and intervention are vital for improving patient outcomes and quality of life, as many individuals with PAD do not receive the care they need. Addressing risk factors proactively can help manage the condition effectively.
How can lifestyle changes impact PAD?
Making lifestyle changes, such as quitting smoking, managing diabetes, controlling blood pressure and cholesterol levels, and increasing physical activity, can reduce the risk of PAD and improve cardiovascular health.
What should individuals do if they experience symptoms of PAD?
If individuals experience symptoms such as leg pain or cramping during physical activities, it is important to seek medical help for proper screening and treatment options.