


Managing congestive heart failure (CHF) is a journey that many face, and medications play a crucial role in this process. Classes such as diuretics, ACE inhibitors, and beta-blockers are not just treatments; they are lifelines that can significantly improve symptoms and enhance patient outcomes. Have you ever wondered how these medications can truly make a difference in your daily life? Effective management involves more than just taking medications; it requires adherence to prescribed treatments, regular monitoring, and thoughtful lifestyle modifications. These steps can lead to a better quality of life.
Evidence from clinical trials shows that these medications are effective in reducing hospitalizations and mortality rates. This is reassuring news for those navigating the challenges of CHF. Remember, you are not alone in this journey. Support is available, and taking action towards your health can lead to positive changes. If you have concerns or questions about your treatment plan, please reach out for guidance. Your well-being is important, and there are resources ready to help you every step of the way.
Understanding congestive heart failure (CHF) can be overwhelming, especially when faced with the many treatment options available. Medications are essential in managing this chronic condition, providing patients with the opportunity for a better quality of life and alleviated symptoms. Yet, the world of heart failure treatments can feel intricate, often leaving patients uncertain about which medications are most effective and how to stick to their prescribed regimens.
What strategies can help individuals take charge of their health and enhance their treatment for CHF?
By exploring available options and seeking support, you can navigate this journey with confidence. Remember, you are not alone in this process, and there are resources and people ready to assist you every step of the way.
Congestive heart failure (CHF) is a long-term condition that can be challenging, as it involves the heart's struggle to pump blood efficiently. This often leads to insufficient circulation to meet the body's needs, causing symptoms such as shortness of breath, fatigue, and fluid retention. These symptoms can significantly affect your quality of life. However, understanding your treatment options can empower you to actively engage in managing your health.
Medications for congestive heart failure are crucial in managing CHF. Commonly prescribed medications for congestive heart failure include:
Recent research highlights the effectiveness of these therapies. For instance, the DAPA-HF trial found that dapagliflozin led to a 26% relative risk reduction in the primary composite outcome among individuals with reduced ejection fraction. Similarly, the EMPEROR-Reduced trial demonstrated a 25% decrease in cardiovascular mortality and heart failure hospital admissions for those receiving empagliflozin.
Real-world outcomes further emphasize the importance of medications for congestive heart failure. In the ADVOR trial, successful decongestion after 72 hours was achieved in 42.2% of individuals treated with acetazolamide, compared to 30.5% in the placebo group. This illustrates the tangible benefits of targeted pharmacotherapy, particularly with medications for congestive heart failure. Additionally, the AFFIRM-AHF trial showed that iron supplementation with ferric carboxymaltose reduced the risk of hospitalizations for heart failure in individuals with ejection fraction <50% and iron deficiency, highlighting the significance of managing comorbid conditions in the context of medications for congestive heart failure treatment.
In addition to pharmacotherapy, Amavita's CardioElite™ program enhances CHF management by providing advanced, real-time diagnostic data and 24/7 cardiology consultation. This comprehensive approach not only aids in treatment management but also enables healthcare providers to proactively address individual needs, ultimately reducing readmissions and improving overall cardiac care. Cardiologists stress that understanding CHF treatments is vital for patients. As one specialist observed, "Empowering patients with information about their treatments can lead to better adherence and enhanced health results." This patient-centered approach is essential for managing CHF effectively and improving overall well-being. Furthermore, nonpharmacological strategies, like limiting sodium and fluid intake, are crucial in managing cardiac insufficiency and should be considered alongside pharmacotherapy.

Managing heart failure can feel overwhelming, but there are several classes of medications that can help ease your symptoms and improve your quality of life. Each type of medication works in its own way, offering distinct benefits that can make a significant difference in your daily comfort.
Diuretics: These essential medications help reduce fluid buildup in your body, alleviating uncomfortable symptoms like swelling and shortness of breath. They are particularly effective in managing congestion, and studies show that using diuretics can lead to notable improvements in comfort and overall quality of life.
ACE Inhibitors: By relaxing your blood vessels, ACE inhibitors promote smoother blood flow, which decreases the workload on your heart and lowers blood pressure. Their effectiveness is well-documented, with real-world examples showing a significant reduction in hospitalizations for those experiencing cardiovascular failure.
Beta-Blockers: These medications work by reducing your pulse rate and lowering blood pressure, which can enhance your heart's function over time. Clinical trials have demonstrated that individuals taking beta-blockers often experience better outcomes, including lower mortality rates.
Mineralocorticoid Receptor Antagonists (MRAs): MRAs play a crucial role in preventing fluid retention and improving heart function, making them an important part of treatment plans for cardiac insufficiency. Their use has been associated with improved survival rates for individuals facing cardiac dysfunction.
Angiotensin Receptor Neprilysin Inhibitors (ARNIs): This newer class of medications combines the effects of an ACE inhibitor and a neprilysin inhibitor, providing additional benefits in managing heart failure. Recent studies suggest that ARNIs can significantly reduce the risk of cardiovascular death and hospitalizations, making them a promising option for many.
While every medication category comes with potential side effects, it’s essential to discuss these with your healthcare provider. They can help ensure that your treatment plan is tailored to your individual needs, enhancing your outcomes and supporting your journey towards better health. Remember, you are not alone in this; support is available to help you navigate your treatment options.

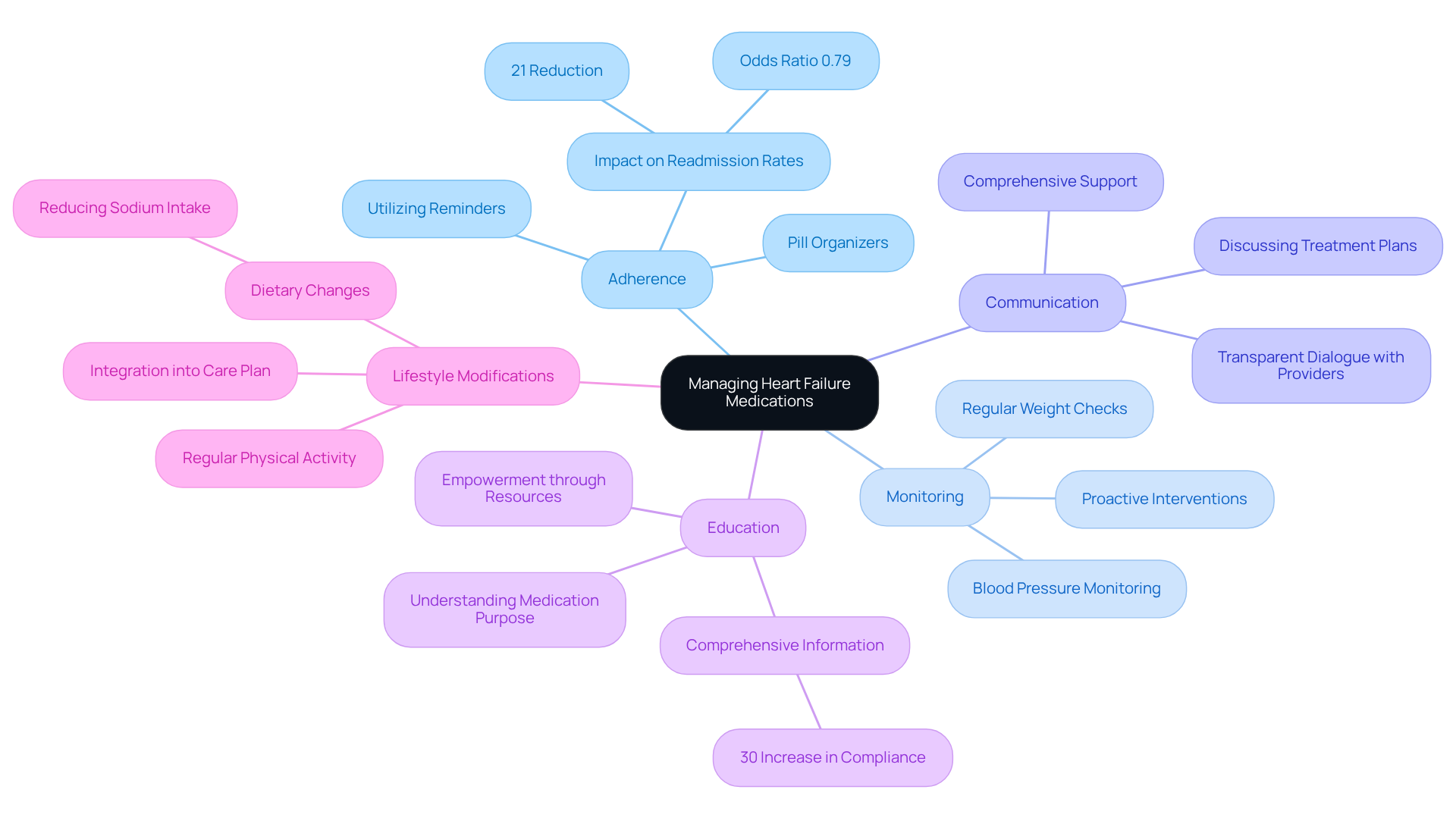
Effectively managing medications for congestive heart failure is crucial for enhancing patient outcomes and quality of life, especially within the supportive framework of Amavita's CardioElite™ program. Here are several best practices to consider:
By adhering to these practices, you can significantly enhance your treatment outcomes and maintain a better quality of life while managing congestive heart failure. Remember, you are not alone in this journey; support is always available.
Understanding the intricacies of medications for congestive heart failure is vital for anyone navigating this challenging condition. Effective medication management not only alleviates symptoms but also enhances overall quality of life for patients. By recognizing the roles of various medications, individuals can take charge of their health and make informed decisions about their treatment options.
Have you considered the importance of adhering to prescribed regimens? Different medication classes, such as:
play significant roles in managing your health. Additionally, comprehensive programs like Amavita's CardioElite™ offer valuable support. These elements collectively underscore the necessity of proactive management strategies, including regular monitoring and open communication with healthcare providers, which can lead to improved health outcomes and reduced hospitalizations.
Ultimately, empowering yourself with knowledge about congestive heart failure and its treatments is crucial. Implementing best practices in medication management, alongside lifestyle modifications, can significantly enhance your journey towards better heart health. Remember, it is essential to engage actively in your treatment plans, seek support, and utilize available resources to navigate this condition effectively. You are not alone on this journey; there are people and programs ready to help you every step of the way.
What is congestive heart failure (CHF)?
Congestive heart failure (CHF) is a long-term condition where the heart struggles to pump blood efficiently, leading to insufficient circulation to meet the body's needs. This can cause symptoms such as shortness of breath, fatigue, and fluid retention.
What are the common symptoms of CHF?
Common symptoms of CHF include shortness of breath, fatigue, and fluid retention, all of which can significantly affect the quality of life.
What medications are commonly prescribed for CHF?
Commonly prescribed medications for CHF include diuretics to reduce fluid buildup, ACE inhibitors to relax blood vessels and lower blood pressure, and beta-blockers to decrease the heart's workload and enhance its function.
How effective are medications for treating CHF?
Recent research has shown that medications can significantly improve outcomes for CHF patients. For example, the DAPA-HF trial found a 26% relative risk reduction in adverse outcomes for those taking dapagliflozin, while the EMPEROR-Reduced trial showed a 25% decrease in cardiovascular mortality and heart failure hospital admissions with empagliflozin.
What does the ADVOR trial reveal about CHF treatment?
The ADVOR trial demonstrated that successful decongestion after 72 hours was achieved in 42.2% of individuals treated with acetazolamide, compared to 30.5% in the placebo group, highlighting the benefits of targeted pharmacotherapy.
What role does iron supplementation play in CHF management?
The AFFIRM-AHF trial indicated that iron supplementation with ferric carboxymaltose reduced the risk of hospitalizations for heart failure in individuals with an ejection fraction of less than 50% and iron deficiency, underscoring the importance of managing comorbid conditions.
How does Amavita's CardioElite™ program assist in CHF management?
Amavita's CardioElite™ program enhances CHF management by providing advanced, real-time diagnostic data and 24/7 cardiology consultation, which helps healthcare providers proactively address individual patient needs, reduce readmissions, and improve overall cardiac care.
Why is patient education important in managing CHF?
Understanding CHF treatments is vital for patients, as empowering them with information can lead to better adherence to treatment plans and enhanced health outcomes.
Are there non-pharmacological strategies for managing CHF?
Yes, non-pharmacological strategies such as limiting sodium and fluid intake are crucial in managing cardiac insufficiency and should be considered alongside pharmacotherapy.