


Understanding the complexities of cardiac output is essential for anyone who cares about their heart health. This important measurement shows how well the heart pumps blood, delivering vital oxygen and nutrients throughout the body. As more people, especially older adults, face conditions that can lower cardiac output, it becomes increasingly important to recognize the symptoms and underlying causes.
How can you keep an eye on your heart function and ensure you get the help you need to prevent serious health issues? Monitoring your heart health is not just about numbers; it’s about feeling secure and supported in your journey.
In addition to this, being aware of the signs of decreased cardiac output can empower you to take action. Simple steps, like regular check-ups and open conversations with your healthcare provider, can make a significant difference. Remember, you’re not alone in this; there are resources and support systems available to help you navigate your heart health with confidence.
Cardiac performance, or cardiac output (CO), refers to the volume of blood your heart pumps each minute, typically measured in liters. This measurement is crucial as it serves as a vital indicator of your heart's function and overall cardiovascular health. Generally, a healthy heart performs between 4 to 8 liters per minute, but this can vary based on factors like age, body size, and physical condition.
Understanding CO is essential because it reflects your heart's ability to deliver oxygen and nutrients to your body's tissues, which is necessary for sustaining metabolic functions. When blood flow decreases, it can result in decreased cardiac output related to insufficient organ perfusion, potentially causing serious health issues. This is especially concerning for older adults who may already have conditions affecting their cardiovascular health.
At Amavita Heart and Vascular Health®, we recognize the importance of thorough evaluations to assess risk factors and develop personalized strategies aimed at reducing the risk of a heart attack. Our preventive cardiology approach combines advanced risk evaluation tools with tailored interventions, ensuring that elderly patients receive the specialized care they need to maintain optimal cardiac function and overall well-being.
If you have concerns about your heart health, please don’t hesitate to reach out. We’re here to support you every step of the way.

Decreased cardiac output related to various medical conditions can affect the heart's ability to function effectively. Understanding these issues is vital for your health and well-being.
Heart Failure: This condition arises when the heart struggles to pump blood efficiently, often due to weakened muscles or structural issues. Did you know that around 6.7 million Americans over 20 live with heart failure? This number is expected to rise to 10.3 million by 2040. It’s important to recognize this condition early.
Arrhythmias: Irregular heartbeats, especially atrial fibrillation, can disrupt how well your heart pumps. You might notice signs like fatigue, dizziness, or shortness of breath. These symptoms can complicate heart performance, so it’s essential to pay attention to them.
Myocardial Infarction: Damage to the heart muscle from a heart attack can significantly hinder its function. This can lead to reduced performance and an increased risk of heart failure. If you or someone you know has experienced this, seeking help is crucial.
Valvular Heart Disease: When the heart valves don’t work properly, they can obstruct blood flow, making it harder for your heart to perform well. Regular check-ups can help catch these issues early.
Hypovolemia: Conditions that lead to low blood volume, like dehydration or significant bleeding, can decrease the amount of blood available for your heart to pump. This directly impacts circulation, so staying hydrated is key.
Sepsis: Severe infections can cause systemic vasodilation and reduce venous return, which decreases heart function and can lead to serious complications. If you notice signs of infection, don’t hesitate to seek medical attention.
Recognizing these causes is essential for developing effective management and treatment strategies. Recent studies highlight that amyloidosis, often mistaken for high blood pressure or aging, is an underacknowledged factor in heart failure and reduced blood circulation. Timely identification and action can greatly enhance outcomes for individuals. Remember, awareness and education are vital in managing your cardiovascular wellness. If you have concerns, please reach out for support. You’re not alone in this journey.

Symptoms of decreased cardiac output can show up in various ways, and it’s important to recognize them. Fatigue and shortness of breath are particularly significant indicators. Persistent tiredness often stems from inadequate oxygen delivery to your tissues, making even everyday activities feel exhausting. In fact, research shows that nearly 80% of individuals with cardiac failure report experiencing shortness of breath, especially during physical activity, as their bodies strive to meet increased oxygen demands.
Recognizing fatigue is crucial, as it can signal worsening heart function. You might find yourself struggling to complete routine tasks without feeling overly tired. This symptom often comes with dizziness or lightheadedness, which can happen due to insufficient blood flow to the brain.
Another common symptom is swelling, or edema, in the legs, ankles, or abdomen, resulting from fluid retention due to decreased cardiac output related to heart function. You may also experience chest discomfort, which can indicate underlying cardiovascular issues or ischemia, along with cold extremities due to poor circulation.
It’s also important to keep an eye on weight changes. A weight increase of over 2-3 pounds in a single day or 5 pounds in a week could signal worsening cardiac failure. Early recognition of these symptoms is vital, as it can lead to necessary evaluations and interventions. At Amavita, individuals at higher risk, including those with diabetes, hypertension, or a family history of cardiovascular issues, can benefit from advanced imaging methods like echocardiograms and cardiac MRIs, which provide detailed insights into heart function. These comprehensive evaluations ensure effective treatment monitoring and personalized care. Management options may include supplemental oxygen and medications to enhance heart function.
By monitoring changes in fatigue levels and shortness of breath, you can lead yourself to timely medical consultations, ultimately improving your outcomes and quality of life. Remember, you’re not alone in this journey; support is available, and reaching out can make a significant difference.

Evaluating and diagnosing reduced heart output is a journey that healthcare providers take with you, ensuring that every step is precise and compassionate. Here are some key methods they use:
These thorough evaluations are essential for understanding the reasons behind decreased cardiac output related to reduced heart function. They allow healthcare professionals to tailor treatment strategies just for you, ensuring you receive the best possible care. Remember, you’re not alone in this; support is always available.

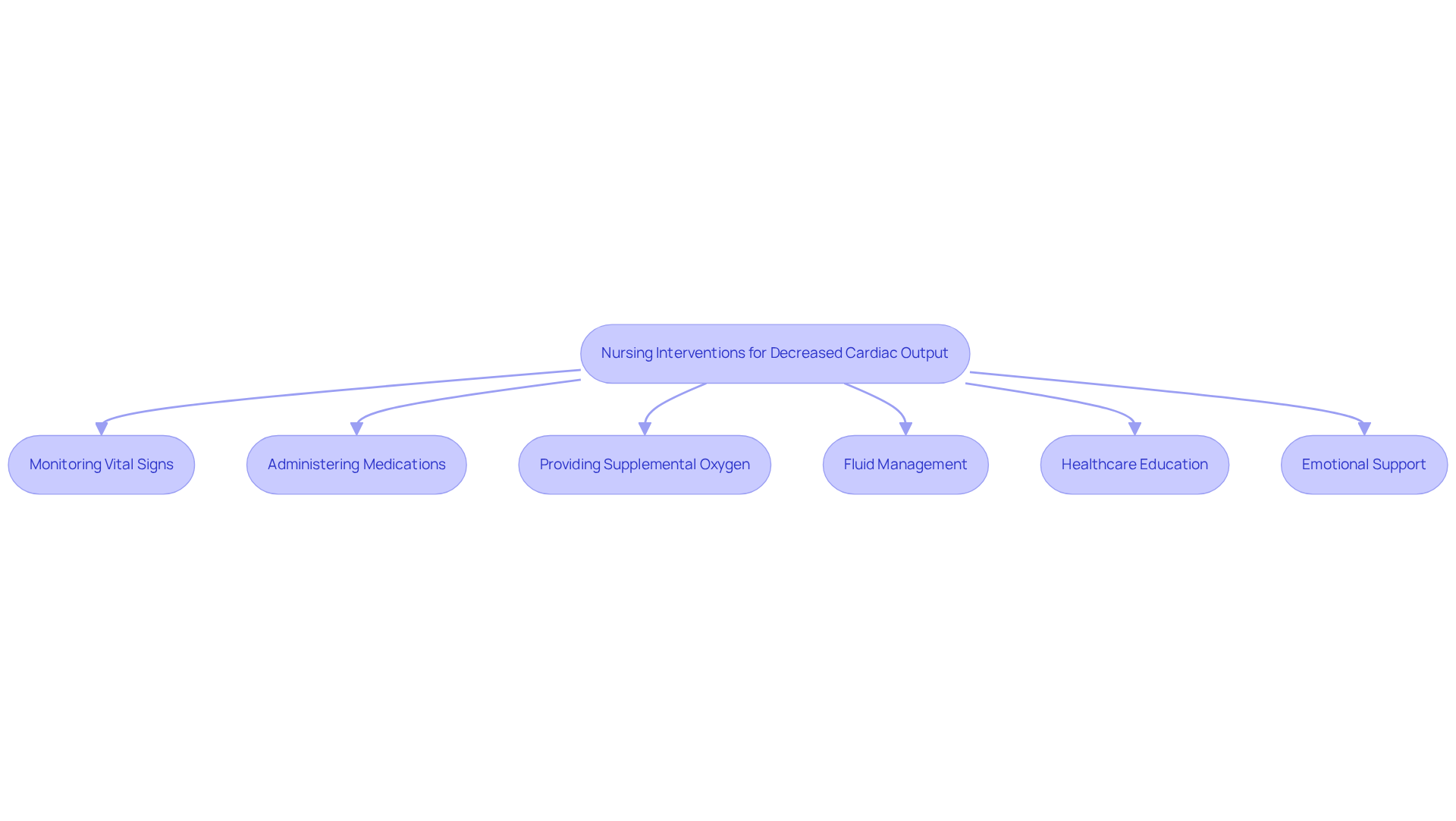
Nursing interventions for patients experiencing decreased cardiac output related to their condition are essential for their well-being.
Monitoring vital signs is a crucial first step. Regularly checking heart rate, blood pressure, and oxygen saturation helps us detect any changes, especially in high-risk patients like the elderly who may have conditions such as diabetes or hypertension.
Administering medications tailored to individual needs is another vital intervention. This may include diuretics to alleviate fluid overload or inotropes to enhance heart contractility. At Amavita, we focus on customizing treatment to ensure the best outcomes for each patient.
Providing supplemental oxygen is also important. It enhances the oxygen supply to tissues, which is vital for those facing cardiac challenges.
Additionally, fluid management plays a key role. By monitoring intake and output, we can prevent fluid overload and provide comprehensive care that addresses specific cardiovascular risks.
Healthcare education is a cornerstone of our approach. We guide individuals on lifestyle adjustments, including dietary changes and physical activity, to promote heart health. This personalized strategy is crucial for our patients at Amavita.
Moreover, emotional support is integral to our care. We understand that tackling anxiety and offering reassurance to patients and their families is essential. Mental wellness is a significant aspect of heart care, and we are here to support you.
Implementing these interventions can significantly enhance the quality of care and improve outcomes for patients with decreased cardiac output related to their condition.
With the advanced imaging and comprehensive evaluations offered at Amavita Heart and Vascular Health, you can feel confident in the support and expertise we provide.
Understanding decreased cardiac output is crucial for maintaining heart health and overall well-being. Have you ever wondered how your heart is performing? This article highlights the significance of cardiac output as a vital measure of heart performance, emphasizing its role in delivering essential oxygen and nutrients to your body's tissues. Recognizing the implications of reduced cardiac output and its associated conditions can empower you to take proactive steps in managing your heart health.
Key insights discussed include the various causes of decreased cardiac output, such as:
Symptoms like fatigue, shortness of breath, and edema serve as critical indicators that require timely attention. Diagnostic tools, including:
play a pivotal role in assessing heart function, enabling healthcare providers to develop personalized care plans tailored to your needs. Furthermore, effective nursing interventions and ongoing education are essential to support you in your journey toward improved heart health.
Ultimately, awareness and proactive management of decreased cardiac output can significantly enhance your quality of life. It’s important to stay informed about your heart health, recognize symptoms early, and seek professional guidance when necessary. By prioritizing heart health and understanding the factors that influence cardiac output, you can take meaningful steps toward a healthier future. Remember, you are not alone in this journey; support is always available.
What is cardiac output and why is it important?
Cardiac output (CO) is the volume of blood the heart pumps each minute, typically measured in liters. It is crucial as it indicates the heart's function and overall cardiovascular health, reflecting its ability to deliver oxygen and nutrients to the body's tissues.
What is the normal range for cardiac output?
A healthy heart typically performs between 4 to 8 liters per minute, though this can vary based on factors like age, body size, and physical condition.
What can happen if cardiac output decreases?
A decrease in cardiac output can lead to insufficient organ perfusion, resulting in serious health issues, particularly for older adults with existing cardiovascular conditions.
What are some common causes of decreased cardiac output?
Common causes include heart failure, arrhythmias, myocardial infarction, valvular heart disease, hypovolemia, and sepsis.
What is heart failure?
Heart failure occurs when the heart struggles to pump blood efficiently, often due to weakened muscles or structural issues. It affects approximately 6.7 million Americans over 20 and is expected to rise significantly by 2040.
How do arrhythmias affect cardiac output?
Arrhythmias, such as atrial fibrillation, can disrupt the heart's pumping efficiency, leading to symptoms like fatigue, dizziness, or shortness of breath, which complicate heart performance.
What impact does a myocardial infarction have on the heart?
A myocardial infarction, or heart attack, damages the heart muscle, significantly hindering its function, which can lead to reduced performance and an increased risk of heart failure.
How does valvular heart disease affect cardiac output?
Valvular heart disease occurs when the heart valves do not function properly, obstructing blood flow and making it harder for the heart to perform effectively.
What is hypovolemia and how does it impact the heart?
Hypovolemia is a condition characterized by low blood volume due to dehydration or significant bleeding, which decreases the amount of blood available for the heart to pump, directly impacting circulation.
What role does sepsis play in decreased cardiac output?
Sepsis, a severe infection, can cause systemic vasodilation and reduce venous return, which decreases heart function and can lead to serious complications.
Why is it important to recognize the causes of decreased cardiac output?
Recognizing the causes is essential for developing effective management and treatment strategies, which can significantly enhance health outcomes for individuals with cardiovascular issues.