


Understanding the unique presentation of cardiac symptoms in women is crucial, especially as they age and face heightened risks associated with heart disease. Women often experience heart-related issues differently than men, with subtler signs that can lead to misdiagnosis and delayed treatment. As the prevalence of cardiovascular disease increases post-menopause, recognizing these symptoms becomes paramount.
How can elderly women ensure they are not overlooked in a healthcare system that often defaults to male-centric models of heart health? It’s essential to advocate for oneself and seek clarity when something feels off. Remember, your health matters, and you deserve to be heard.
In addition to this, consider discussing any unusual symptoms with your healthcare provider. They can help you navigate your concerns and ensure you receive the appropriate care. You are not alone in this journey; support is available, and taking action can lead to better health outcomes.
Heart conditions show distinct traits in women, shaped by biological and hormonal factors. Typically, women face cardiovascular issues later in life, often after menopause, when estrogen levels drop significantly, increasing cardiovascular risk. This hormonal shift is vital; a lack of estrogen can lead to problems like endothelial dysfunction and increased arterial stiffness, both of which are key contributors to heart issues.
Moreover, women generally have smaller coronary arteries, which can make detecting and treating blockages more challenging. Cardiac symptoms in women can also differ greatly from those in men when it comes to heart disease. While men often report classic signs like chest pain, the cardiac symptoms in women may include more subtle indicators such as fatigue, shortness of breath, or gastrointestinal discomfort. This difference in symptom presentation highlights the importance of awareness and understanding of cardiac symptoms in women, particularly among older women who might not display traditional symptoms.
Research shows that postmenopausal women face a two- to six-fold higher risk of cardiovascular disease compared to their premenopausal counterparts. This underscores the urgent need for tailored cardiovascular health strategies. At Amavita Heart and Vascular Health®, we believe in a comprehensive approach to cardiac care. We utilize advanced imaging and testing all in one location to ensure accurate diagnosis without delay.
Our CardioElite™ system, powered by AISAP's FDA-approved AI ultrasound diagnostic platform, enhances our diagnostic capabilities. It allows for real-time analysis and immediate insights into cardiovascular structure and function. Our preventive cardiology strategy combines advanced risk evaluation tools with personalized interventions, significantly reducing the risk of heart attacks.
As Monica Potter wisely stated, "heart disease is the No. '1 killer of American females," emphasizing the urgent need for awareness and proactive measures. Recognizing these unique features is essential for ensuring timely diagnosis and effective treatment, ultimately improving health outcomes for women. Remember, you are not alone in this journey; we are here to support you every step of the way.

Women often experience cardiac symptoms in women that can be quite different from what’s typically associated with men. It’s crucial to recognize these signs, which may include:
Recognizing cardiac symptoms in women is essential. Research indicates that cardiac symptoms in women are often misdiagnosed during heart attacks, leading to many facing delays in treatment. Often, women describe their pain, including cardiac symptoms in women, in ways that are less recognizable, increasing the chances of misdiagnosis.
At Amavita Heart and Vascular Health®, we understand these concerns and emphasize the importance of thorough cardiac evaluations and preventive strategies to address cardiac symptoms in women. Our advanced imaging capabilities and personalized interventions are designed to address these issues effectively.
It’s essential for patients, especially those at high risk, to advocate for themselves in medical settings when experiencing cardiac symptoms in women. Dr. Reynolds reminds us, "If you’re experiencing symptoms, don’t hesitate to speak up. Go to the emergency department, and let healthcare providers know you believe you’re having a cardiac event for prompt diagnosis and treatment."
Prompt medical attention is crucial if there are any cardiac symptoms in women that are suspected. Remember, timely intervention can significantly improve outcomes. You are not alone in this journey; we are here to support you every step of the way.

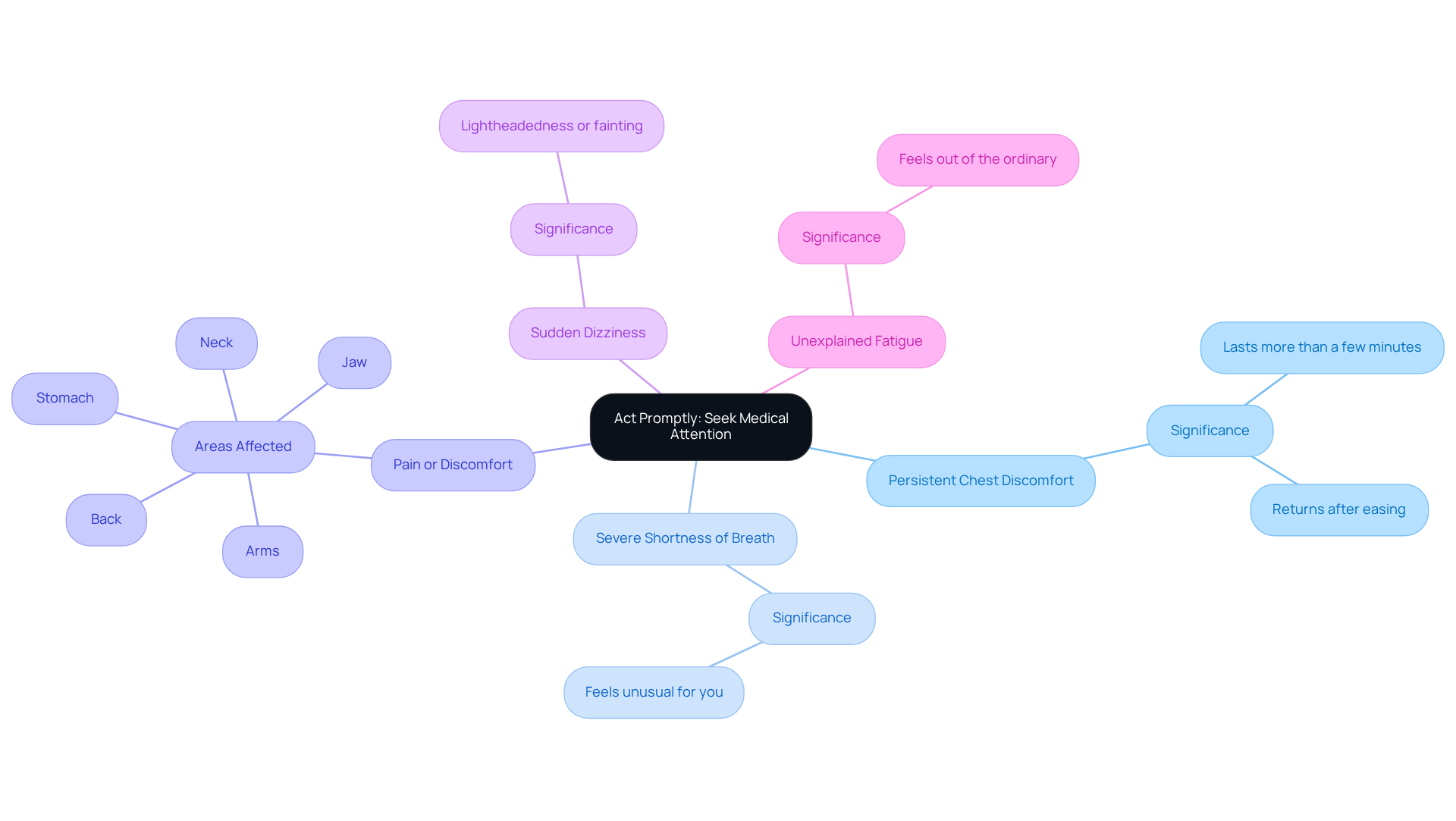
Elderly women, it's important to pay attention to your body. If you notice any of these symptoms, please seek medical help right away:
Taking timely action can make a big difference. Studies show that early intervention significantly improves outcomes for those facing cardiovascular issues. It's crucial to recognize that women often experience atypical cardiac symptoms, which can lead to delays in receiving the care they need. Cardiologists stress that being aware of these signs and acting quickly is vital, as prompt medical attention can greatly improve your prognosis.
Did you know that women are twice as likely as men to experience serious cardiac symptoms? This often happens because the cardiac symptoms in women are misunderstood. Additionally, around 170,000 of the 805,000 cardiovascular incidents each year are considered silent, which highlights how common unrecognized cardiac symptoms in women are, especially.
At Amavita Heart and Vascular Health®, we’re here to support you. Our advanced AI-driven diagnostic technology uses a portable, FDA-approved ultrasound that provides real-time assistance for accurate imaging. You’ll receive reports on your cardiac structure and function within minutes, allowing for timely interventions.
Our AHA certification reflects our dedication to high-quality care, enhancing the trust you can place in our services and helping to reduce hospital readmissions. Understanding and responding to these important signs is essential for improving survival rates and overall cardiovascular health. Remember, you’re not alone in this journey; we’re here to help you every step of the way.
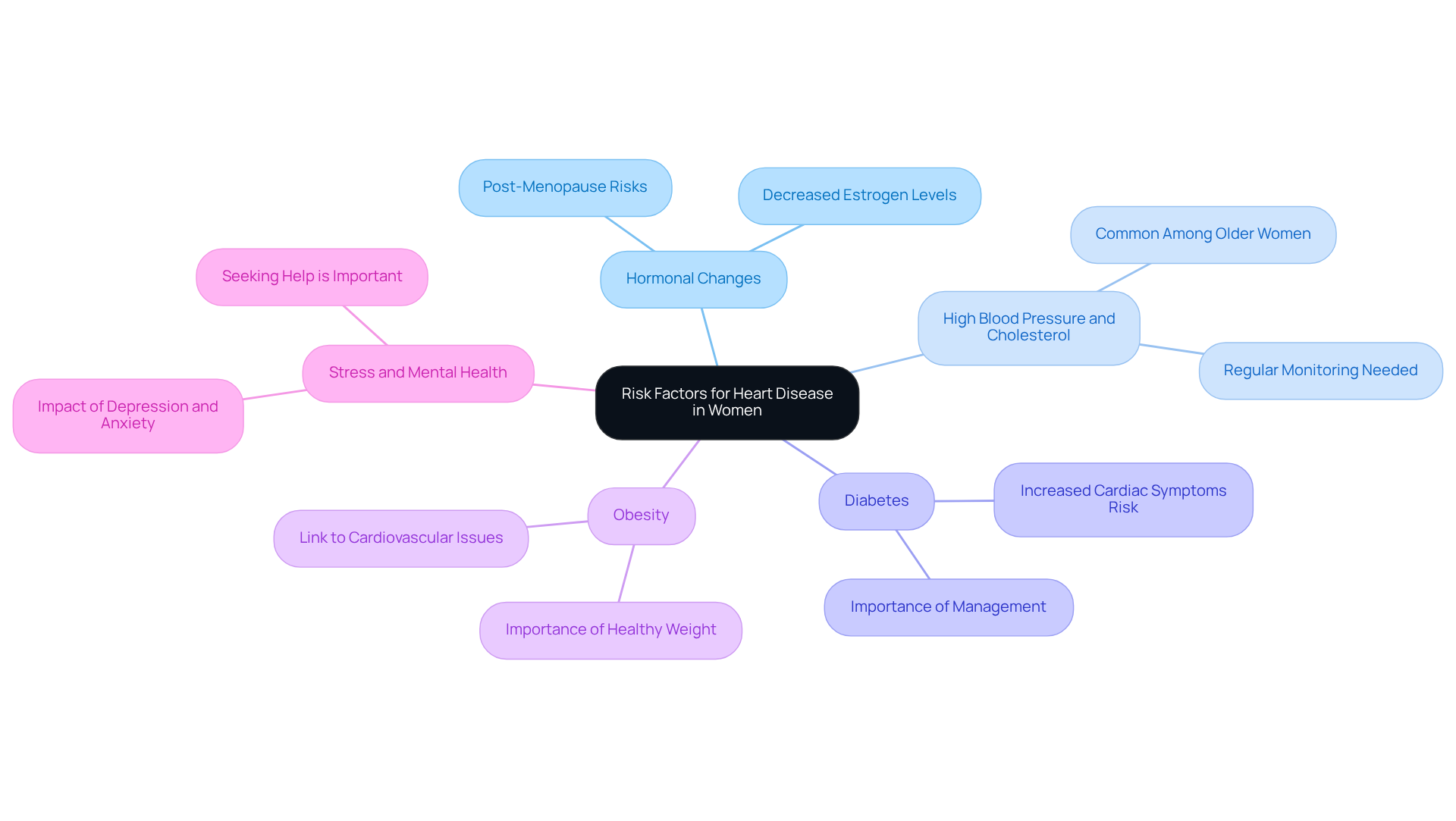
As women age, several risk factors can significantly contribute to heart disease, and it’s important to understand these to take proactive steps for better health:
Hormonal Changes: After menopause, many women experience a notable increase in cardiovascular risk due to decreased estrogen levels, which are vital for heart health. This shift can make women more vulnerable to cardiac symptoms in women, and recognizing this change is the first step towards care.
High Blood Pressure and Cholesterol: Elevated blood pressure and cholesterol levels are significant contributors to heart conditions. Research shows that these issues are common among older women, making regular monitoring and management essential to reduce risks. Have you had your levels checked recently?
Women with diabetes face an even greater risk of experiencing cardiac symptoms in women compared to men. This emphasizes the importance of effective diabetes management as a crucial aspect of a comprehensive approach to understanding cardiac symptoms in women. Taking control of diabetes can make a real difference.
Obesity: Carrying excess weight is a major factor in cardiovascular issues. Obesity is linked to various complications related to the circulatory system, so maintaining a healthy weight is crucial for lowering the risk of heart disease. Small changes can lead to significant improvements.
Stress and Mental Health: Psychological factors, such as depression and anxiety, can elevate the risk of cardiovascular disease in women. Addressing mental health is just as important as physical health for overall well-being. Remember, it’s okay to seek help.
Understanding these factors empowers women to take preventive measures and seek appropriate care for cardiac symptoms in women. You’re not alone in this journey, and reaching out for support can enhance your heart health and overall quality of life.
Understanding the unique aspects of heart disease in women, especially among elderly patients, is vital for improving health outcomes. Have you ever considered how hormonal changes and biological differences can affect your heart health? It’s important to recognize that symptoms in women can often present more subtly, complicating diagnosis and treatment. By raising awareness and educating ourselves about these factors, we empower women to advocate for their health and seek timely medical attention.
Key insights include:
Ultimately, understanding cardiac symptoms in women is more than just awareness; it’s a call to action for both patients and healthcare providers. By prioritizing education and timely intervention, we can navigate the journey toward better cardiovascular health together. Women must feel empowered to communicate their symptoms and seek help, ensuring they receive the care they need. Together, these steps can significantly enhance the quality of life and survival rates for women facing heart disease.
How does heart disease manifest differently in women compared to men?
Heart disease in women often presents with more subtle symptoms such as fatigue, shortness of breath, or gastrointestinal discomfort, rather than the classic chest pain commonly reported by men.
What biological factors contribute to the increased cardiovascular risk in women?
Women typically face cardiovascular issues later in life, particularly after menopause when estrogen levels drop. This hormonal shift can lead to endothelial dysfunction and increased arterial stiffness, both of which contribute to heart problems.
Why is it challenging to detect and treat heart disease in women?
Women generally have smaller coronary arteries, which can complicate the detection and treatment of blockages. Additionally, their cardiac symptoms may differ from the traditional signs associated with heart disease.
What is the increased risk of cardiovascular disease for postmenopausal women?
Research indicates that postmenopausal women face a two- to six-fold higher risk of cardiovascular disease compared to their premenopausal counterparts.
What approach does Amavita Heart and Vascular Health® take towards cardiac care for women?
Amavita Heart and Vascular Health® employs a comprehensive approach, utilizing advanced imaging and testing for accurate diagnosis, along with the CardioElite™ system for enhanced diagnostic capabilities and personalized preventive cardiology strategies.
What is the significance of awareness regarding heart disease in women?
Increased awareness is crucial as heart disease is the leading cause of death among American females. Recognizing the unique features of heart disease in women can lead to timely diagnosis and effective treatment, improving health outcomes.
How can women seek support in their heart health journey?
Women are encouraged to reach out for support and utilize the resources available at facilities like Amavita Heart and Vascular Health®, which are dedicated to providing comprehensive cardiac care tailored to women's needs.