


Florida's Skilled Nursing Facilities (SNFs) face a critical challenge: a revolving door of cardiac patient readmissions that cost the state's healthcare system billions, strain resources, and jeopardize patient health.(1) With 30-day readmission rates for heart failure patients as high as 43% and a one-year mortality rate over 50%, the traditional model of post-acute care is failing.(2) In response, amavita CardioElite™ offers a groundbreaking solution. As the first program of its kind, CardioElite™ integrates bedside AI-powered diagnostics, a guided pathway to elite American Heart Association (AHA) certification, and comprehensive staff training to empower SNFs.(2) This report details how the CardioElite™ program directly confronts the readmission crisis, offering a data-driven blueprint for SNFs to achieve superior clinical outcomes, generate immediate ROI, and become recognized leaders in cardiovascular care.(2)
For too many of Florida's Skilled Nursing Facilities (SNFs), the journey of a post-acute cardiac patient has become a predictable and perilous cycle. A patient is discharged from the hospital, arrives at the SNF for rehabilitation, and within weeks—or even days—an emergent event triggers a costly and disruptive transfer back to the hospital. This "revolving door" phenomenon is more than an operational headache; it represents a fundamental breakdown in the continuum of care. It exposes the most vulnerable patients to increased risks, places immense strain on clinical staff, and triggers significant financial repercussions for both hospitals and their post-acute partners.
The scale of this challenge is staggering. Nationally, the cost of unplanned hospital readmissions for Medicare patients exceeds $26 billion annually, with a significant portion of this expenditure driven by cardiovascular conditions.(1) This is not a distant federal accounting issue; it is a direct threat to the financial stability of healthcare providers on the ground. The problem is particularly acute in the Sunshine State. Florida's hospitals are penalized for excess readmissions at a rate that surpasses the national average, creating a powerful incentive for them to scrutinize the performance of their SNF partners.(1) In this high-stakes environment, the ability of an SNF to effectively manage complex cardiac patients is no longer a value-added service; it is a core requirement for survival and growth.
Out of this crisis emerges a transformative solution, born from clinical expertise and technological innovation in Miami. amavita CardioElite™ is not an incremental improvement on a failing system. It is a complete paradigm shift in post-acute cardiovascular management.(2) As the nation's first program to integrate bedside, AI-powered diagnostics with elite American Heart Association certification pathways and comprehensive staff education, CardioElite™ is engineered to do what the traditional model cannot: break the cycle of readmission at its source. This report provides an exhaustive analysis of the cardiovascular care crisis facing Florida's SNFs and details how the CardioElite™ program offers a data-driven, evidence-based blueprint for achieving superior clinical outcomes, unparalleled financial returns, and a new status as a regional leader in cardiac care.
To fully grasp the opportunity that CardioElite™ represents, one must first understand the depth of the problem it solves. The current model for managing post-acute cardiac patients in SNFs is not just inefficient; it is clinically and financially unsustainable. An examination of the data, from the national level down to the specific challenges within Miami-Dade County, reveals a system under immense pressure and ripe for disruption.
The journey of a cardiac patient into a post-acute setting is fraught with inherent risk. Nationally, approximately one in four older patients hospitalized with heart failure (HF) is discharged to an SNF, placing a significant portion of this high-acuity population into a non-hospital environment.(2) This transition marks the beginning of a statistically dangerous period for both the patient and the healthcare system.
The numbers paint a grim picture. For heart failure patients residing in SNFs, the 30-day hospital readmission rate ranges from a troubling 27% to an alarming 43%.3 This means that for every three patients an SNF accepts, at least one is likely to return to the hospital within a month. This cycle of admission and readmission is not only detrimental to patient health but also carries a devastating prognosis. The one-year mortality rate for cardiac patients in SNFs stands at a staggering 53.5%, underscoring the life-or-death importance of effective management in this setting.(2)
Each of these readmissions carries a substantial financial burden. The average cost of a single cardiovascular-related hospitalization is estimated to be between $15,200 and $16,000.(2) For an SNF, facilitating even a handful of these preventable transfers can translate into tens of thousands of dollars in associated costs and lost revenue. At the same time, the referring hospital contributes to a negative performance record with Medicare. Heart failure is not a fringe issue; it is the second leading cause of readmissions for Medicare beneficiaries, making it a primary focus for federal cost-containment and quality improvement initiatives.(8) These national statistics establish a clear baseline: managing cardiac patients in SNFs is a high-risk, high-cost endeavor where the traditional approach is demonstrably failing.
The national trends in post-acute cardiac care are not just mirrored in Florida; they are amplified. As a state with a large senior population, Florida sits at the epicenter of the cardiovascular disease challenge. Heart disease is the leading cause of death in the state, responsible for approximately two out of every ten fatalities.(9) This translates into a massive volume of patients flowing through the healthcare system. In 2022 alone, more than 444,000 Floridians were hospitalized for congestive heart failure, with tens of thousands more admitted for heart attacks and coronary artery disease.(10) A significant percentage of these patients were subsequently discharged to SNFs, placing immense pressure on the state's post-acute care infrastructure.
This high prevalence of cardiovascular disease has direct and painful financial consequences for the state's healthcare providers. Under the Centers for Medicare & Medicaid Services (CMS) Hospital Readmissions Reduction Program (HRRP), hospitals with higher-than-expected readmission rates for specific conditions, including heart failure, face significant financial penalties.(11) Florida is among the states with the highest number of hospitals experiencing high readmission rates.(5) In a recent analysis, a striking 80% of eligible hospitals in Florida were penalized by the HRRP, a rate significantly higher than the national average of 66%.(1) The penalties are not trivial; five Florida hospitals received the maximum possible penalty recently—a 3% reduction in their Medicare reimbursements for an entire fiscal year.(12)
This creates a powerful market dynamic. Hospitals in Florida are under intense financial pressure to reduce their readmission rates. As a result, they are actively seeking post-acute partners who can demonstrate a verifiable ability to manage complex cardiac patients and prevent costly returns to the hospital. An SNF that can provide this assurance becomes a preferred, strategic partner, while one that cannot becomes a financial liability.
Drilling down further into amavita's primary service area of Miami-Dade County reveals the local texture of this statewide challenge. In 2023, Miami-Dade County recorded 4,978 deaths from heart diseases, with an age-adjusted death rate of 129.9 per 100,000 population.(13) While this rate is slightly below the overall Florida average of 135.6, the sheer volume of mortality—nearly 5,000 individuals—highlights the immense concentration of high-risk cardiac patients within this single county.
The infrastructure to care for these patients is also a critical factor. According to 2024 data from the Florida Department of Health, Miami-Dade County has 22 designated Skilled Nursing Unit (SNU) beds, which translates to a rate of just 0.8 beds per 100,000 people. This is substantially lower than the rate in other central counties like Duval (5.2), Lake (7.0), Lee (11.4), or Leon (37.1).(14) This relative scarcity of designated SNU beds suggests that the existing facilities must manage a high volume of complex patients, potentially straining resources and underscoring the need for programs to enhance efficiency and care capacity.
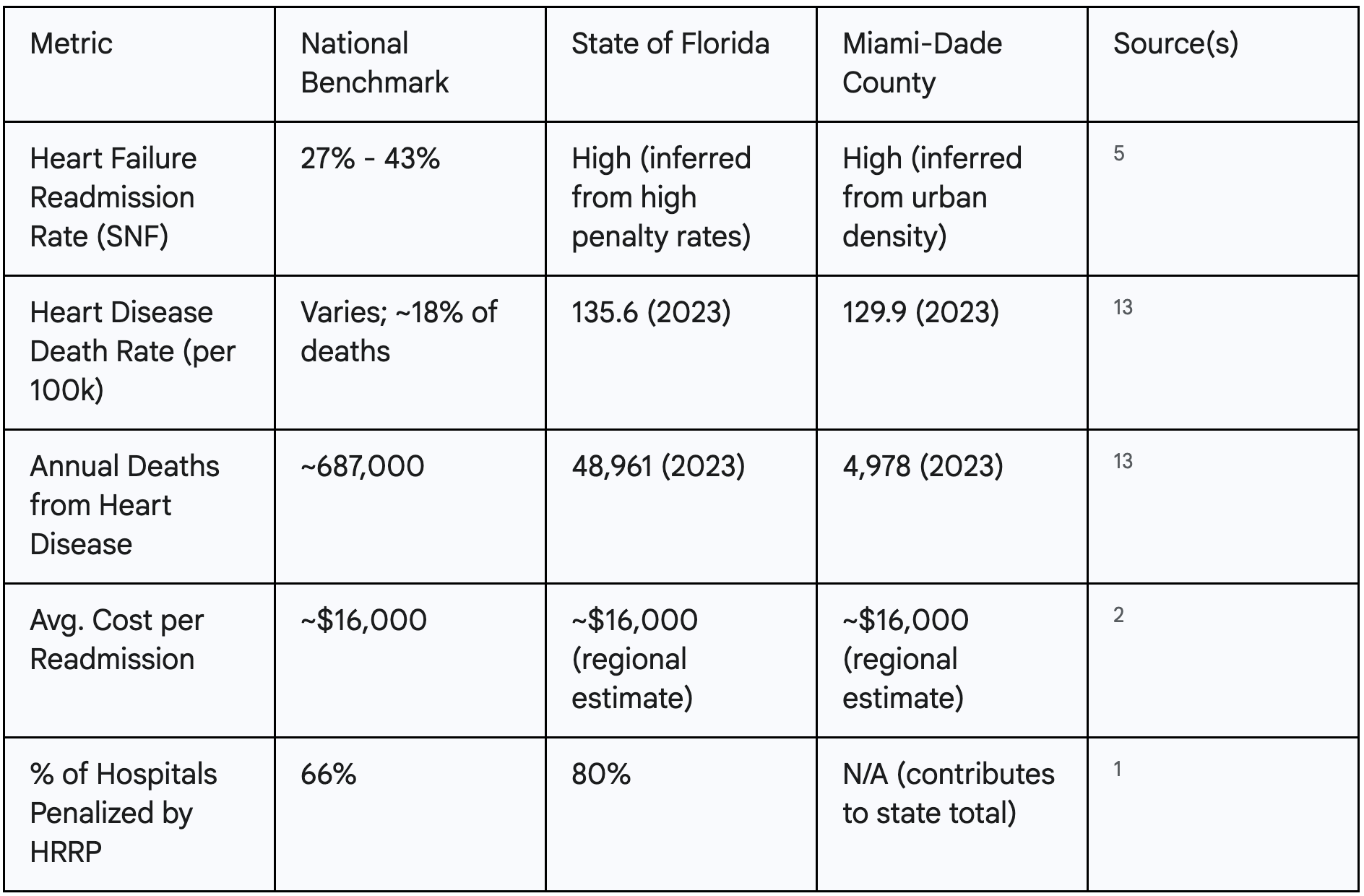
The following table provides a clear, at-a-glance comparison of the cardiac burden, illustrating how the national problem becomes a concrete and urgent business threat for any Florida SNF administrator, particularly in Miami-Dade.
The staggering statistics on readmissions and mortality are not merely a reflection of patient acuity but an indictment of a systemic and operational failure. The data reveals a fundamental mismatch in the post-acute care system: the most clinically complex cardiac patients are routinely discharged to SNFs. This setting is often structurally ill-equipped to manage their needs. This mismatch is the root cause of the revolving door.
Evidence clearly shows that patients discharged to an SNF have inherently higher readmission rates—one study found a 7% readmission rate for SNF-discharged patients compared to just 3% for those sent home.(17) This is the high-risk population that SNFs are expected to manage. Yet, multiple studies and reports highlight the critical capability gaps within many of these facilities. Research indicates that nursing home staff often lack the specialized knowledge and skills required for effective heart failure management, leading to delays in recognizing deteriorating conditions.(19) This is compounded by staffing issues. Lower nursing staff levels are directly correlated with higher hospital readmission rates.(20) In Florida, concerns have been explicitly raised by organizations like AARP about reductions in nursing home staffing standards leading to increased hospitalizations, a clear indicator of declining quality of care.(21)
This confluence of factors—a high-risk patient population entering a resource-constrained environment—creates a predictable outcome. The leading causes of hospital readmissions from SNFs are not surprising; they are symptoms of this underlying systemic flaw. They include poor care coordination between the hospital and the SNF, a lack of patient and family education about the care plan, and a high incidence of medication discrepancies.(22) When a resident's condition changes, an SNF without specialized diagnostic tools or on-site expertise has limited options. The default, risk-averse decision is to initiate an emergency transfer to the hospital, perpetuating the cycle. Readmission, therefore, is not an anomaly; it is the logical and expected result of placing vulnerable patients in an environment without the tools or training to succeed.
In response to the systemic failures of the traditional model, amavita has engineered a new architecture for post-acute cardiovascular care. The CardioElite™ program is not a single product or service but a comprehensive, multi-pillar system designed to directly address and resolve the critical points of failure identified in the data. By integrating advanced technology, elite certification, and deep clinical training, CardioElite™ rebuilds the SNF's cardiac care capabilities from the ground up, transforming it from a passive recipient of high-risk patients into a proactive, data-driven center of excellence.
The cornerstone of the CardioElite™ program is a fundamental shift in diagnostic capability, moving it from the hospital to the patient's bedside. This is accomplished through an exclusive partnership with AISAP, deploying its FDA-cleared AI-powered ultrasound platform directly within the SNF.(2) This technology empowers the facility's nursing staff to conduct point-of-care cardiac diagnostics, a capability previously unimaginable in a post-acute setting.
The contrast between the old way of managing a patient and the CardioElite™ method illustrates the program's transformative power.
This technology acts as a powerful "clinical force multiplier." The healthcare system faces a well-documented shortage of specialized physicians and nurses, a problem acutely felt in the post-acute sector.(22) Furthermore, research has confirmed that SNF staff often lack the specific training needed for complex cardiac care.(19) The CardioElite™ program addresses this foundational challenge not by attempting the impossible task of placing a cardiologist in every SNF, but by upskilling the existing nursing workforce with intelligent technology. It effectively democratizes access to high-level diagnostics, embedding a virtual cardiology consultant at the bedside. This approach solves the critical "knowledge and resource gap" with a scalable, efficient, and technologically advanced solution.
While technology provides the tools, credibility offers the proof. The second pillar of the CardioElite™ program is a guided pathway for partner facilities to achieve official Heart Failure and Stroke Certification from the American Heart Association.(2) This critical differentiator elevates a facility far beyond its peers. An AHA certification is not a simple marketing plaque; it is a rigorous, third-party validation of a facility's commitment to the highest evidence-based care standards, recognized and respected by clinicians, hospital systems, and patients alike.(23)
For an SNF administrator in the competitive Florida market, the strategic benefits of this certification are profound and multi-faceted:
Technology and certification are powerful but only effective when supported by a knowledgeable and confident clinical team. The third pillar of CardioElite™ is a comprehensive, ongoing cardiovascular education program for the entire nursing and clinical staff.(2) This component is designed to directly remedy the staff knowledge gaps that are a documented contributor to poor patient outcomes and high readmission rates in the SNF setting.(19)
This is not a one-time webinar or a simple protocol review. This foundational educational program builds a true culture of cardiovascular competence within the facility. The training equips staff with the advanced skills and clinical judgment to care for high-acuity cardiac patients. This includes a deep understanding of heart failure pathophysiology, recognition of subtle signs of decompensation, and mastery of the essential evidence-based care protocols for preventing crises.
The impact of this pillar extends beyond immediate patient care. By investing in the professional development of its staff, an SNF can significantly improve team morale, clinical confidence, and job satisfaction. This can lead to reduced staff stress and lower turnover rates—a critical operational and financial metric for any SNF, and one that is now being incorporated into CMS's value-based purchasing calculations.(24) This pillar ensures that the team is not just trained to
use the AI-diagnostic tools from Pillar I, but to understand the clinical context behind the data they provide. This synthesis of human expertise and technological power enables a truly superior level of care.
The credibility of the CardioElite™ program is anchored by the deep expertise of its clinical leader, Dr. Pedro Martinez-Clark.(2) A program of this ambition requires a visionary with a proven track record, and Dr. Martinez-Clark's credentials provide an unimpeachable foundation of trust. As a Harvard-trained interventional cardiologist, he brings over 27 years of frontline clinical experience to the program's design and oversight.
His expertise is not merely academic. Having performed over 12,000 minimally invasive cardiovascular procedures, Dr. Martinez-Clark possesses a profound, practical understanding of cardiac disease management. His board certifications in three specialties—Interventional Cardiology, Cardiovascular Disease, and Internal Medicine—reflect a comprehensive grasp of the patient's clinical journey.(2)
Dr. Martinez-Clark is not just an expert in cardiology; he is a pioneer in the technology that powers the CardioElite™ program. His role in spearheading the implementation of the AISAP technology for point-of-care cardiac diagnostics demonstrates that the program is not based on theoretical concepts, but on tools and processes that have been vetted and proven in real-world clinical practice.(2) This direct, hands-on experience ensures that every facet of the CardioElite™ blueprint—from the technology to the training protocols—is grounded in the highest clinical efficacy and practicality standards. The program is not just a vendor solution for SNF partners but a clinical partnership guided by one of the field's leading authorities.
A program's architecture is only as valuable as the results it produces. The CardioElite™ model is not built on speculation but on a foundation of evidence demonstrating its profound impact on clinical outcomes and financial performance. The data provides a clear verdict: this new approach to SNF cardiology successfully slashes readmission rates, generates a significant and immediate return on investment, and strategically positions facilities for success in the new era of value-based healthcare.
The ultimate measure of any clinical program is its ability to improve patient health and safety. The model underpinning the CardioElite™ program, which leverages virtual cardiovascular consultations and advanced diagnostics in the SNF setting, has been the subject of clinical research with dramatic results. The findings from a 2021 peer-reviewed study published in JMIR Cardio, which evaluated a virtual care program for SNF patients, provide a powerful validation of this approach.(3)
The study observed significantly lower hospital readmission rates among patients who received virtual cardiovascular care compared to the expected baseline rates for this high-risk population. The results were striking:
It is critical to recognize the source and significance of these figures. These are not internal marketing projections. The outcomes are published in a reputable, peer-reviewed medical journal, lending them credibility and scientific validity that is rare in the post-acute care industry.(3) By building the CardioElite™ program on this proven, evidence-based model, amavita offers its partners a solution whose efficacy is supported by independent research. This transparent, data-first approach demonstrates a commitment to delivering measurable clinical improvements.
A sound financial case for an SNF administrator must accompany superior clinical outcomes. The CardioElite™ program is designed to deliver an immediate and substantial return on investment by directly targeting the most significant cost driver in post-acute care: preventable hospital readmissions.
The program's financial impact is derived from a precise and conservative calculation based on the clinical results. The "$860 cost savings per patient" figure is not an arbitrary number; it is the product of a straightforward analysis of the value created by preventing readmissions (2):
While this per-patient figure is compelling, the program's financial power becomes evident when scaled to a facility's actual census. The potential for six-figure annual savings is not a remote possibility but a direct projection from the evidence. To help administrators visualize this impact for their facility, the following table provides a simple tool to project the potential return on investment.

This model demonstrates that by investing in proactive, preventative care, an SNF can shift significant funds from the "expense" column of reactive emergency transfers to the "revenue" or "profit" column of its ledger. The ROI is not only positive; it is immediate and grows directly from the facility's commitment to managing this patient population.
The financial benefits of CardioElite™ extend far beyond the direct savings from avoided readmissions. The program is fundamentally designed to align a skilled nursing facility with the dominant and irreversible trend in healthcare: the shift from fee-for-service to value-based care. The volume of services provided does not measure success in this new landscape, but by the quality of patient outcomes achieved.
CMS programs like the Value-Based Purchasing (VBP) initiative and the Hospital Readmissions Reduction Program (HRRP) drive this shift.(2) These programs directly link a provider's reimbursement to its performance on key quality metrics, with readmission rates being a central focus. For SNFs, this presents both a threat and an opportunity.
The threat is clear: hospitals will see an SNF that contributes to high hospital readmission rates as a poor partner, jeopardizing its referral streams. The opportunity, however, is far greater. By implementing the CardioElite™ program, an SNF can fundamentally change its relationship with its referring hospitals. It moves from being a potential source of a hospital's financial penalties to becoming a key part of the solution.
Consider the strategic conversation this enables. An SNF administrator armed with CardioElite™ can approach a hospital's leadership team with a data-backed, financially compelling value proposition: "Your hospital is being penalized for cardiac readmissions. Our facility has invested in an evidence-based, AI-powered cardiology program that has been shown to reduce cardiac readmissions by 70%. By making our facility your preferred partner for post-acute cardiac patients, you can directly mitigate your CMS penalty risk and improve your quality scores."
This transforms the SNF from a simple downstream vendor into an indispensable strategic asset. In a competitive market like Florida, where hospitals actively seek ways to solve their readmission problem, a CardioElite™-certified facility becomes the logical and most attractive choice. This strategic alignment creates a durable competitive advantage, securing a stable flow of high-acuity referrals and positioning the SNF as a vital, proactive partner in the health system's overall success.
The evidence is conclusive. Florida's skilled nursing facilities are at the nexus of a clinical and financial crisis in post-acute cardiovascular care. The traditional model—characterized by reactive decision-making, gaps in staff expertise, and a lack of specialized diagnostic tools—is demonstrably broken, resulting in unacceptably high rates of hospital readmission, poor patient outcomes, and significant financial strain on the entire healthcare system. The status quo is no longer a viable option for facilities that wish to thrive in the era of value-based care.
amavita CardioElite™ offers the only comprehensive, evidence-based solution designed to dismantle this failing model systematically. It is not a patchwork fix but a new operational blueprint for SNF cardiology. By integrating the three essential pillars—bedside AI-powered diagnostics to enable proactive care, a guided pathway to prestigious AHA certification to prove quality, and deep clinical training to build lasting staff competence—the program provides everything a facility needs to transform its capabilities. This unique combination of exclusive technology, the proven expertise of a clinical leader like Dr. Pedro Martinez-Clark, and comprehensive support is unparalleled in the Florida market.(2)
The results of this model are not theoretical; they are validated by clinical research and translate into a powerful financial return. Slashing cardiac readmissions by up to 70% and all-cause readmissions by 33% delivers immediate cost savings and positions a facility as a strategic partner to penalty-averse hospitals.(3)
The opportunity to lead is now. With limited enrollment available for Q3 2025, the time for decisive action is here.2 By embracing the CardioElite™ program, you are not merely adopting a new service but securing your facility's future.
Ready to revolutionize cardiovascular care at your facility? Transform your facility from a skilled nursing facility that treats cardiac patients into a Cardiovascular Center of Excellence that hospitals prefer. Contact amavita today.