


Understanding the nuances between Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) is essential for effective diagnosis and treatment. Both conditions can significantly affect your quality of life, and their symptoms often overlap, which can be confusing. This article explores the key differences in symptoms between PAD and PVD, offering insights that empower you to recognize warning signs and seek timely medical help.
Have you ever wondered how to differentiate between the leg pain associated with PAD and the swelling typical of PVD? By understanding these distinctions, you can take proactive steps toward better vascular health and engage in informed discussions with your healthcare provider. Remember, you’re not alone in this journey; seeking clarity and support is a vital part of managing your health.
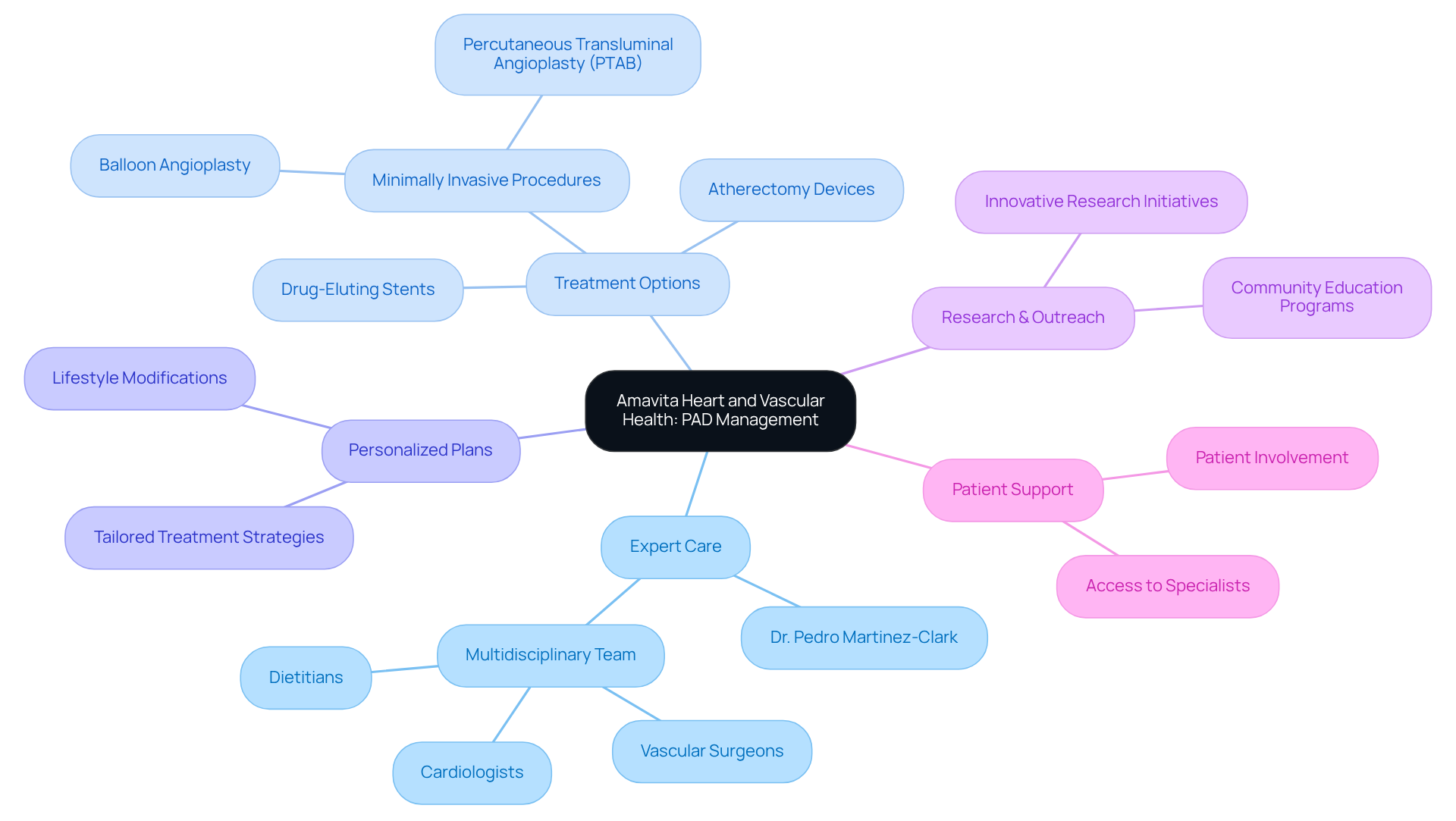
At Amavita Heart and Vascular Health, led by Dr. Pedro Martinez-Clark, we understand the challenges faced by individuals regarding PAD vs PVD symptoms. Our commitment to exceptional cardiovascular care is rooted in compassion and a deep understanding of your needs. We focus on advanced, minimally invasive treatments designed to enhance your recovery and improve your comfort. Each treatment plan is personalized, ensuring that you receive the care that best suits your unique situation.
Managing PAD effectively requires a thoughtful approach. We recognize that addressing both the PAD vs PVD symptoms and the underlying causes is essential. Recent advancements, such as drug-eluting stents and atherectomy devices, have shown promising results in improving blood flow and reducing discomfort. These innovative procedures not only lead to faster recovery times but also minimize the risks associated with traditional surgeries.
Our dedication to your health goes beyond treatment. We actively participate in innovative research and community outreach initiatives, ensuring that you have access to the latest therapies that can significantly enhance your quality of life. By staying informed about advancements in PAD treatment, we aim to address your immediate needs while fostering long-term health and well-being.
If you have concerns about your cardiovascular health, we encourage you to reach out. You are not alone in this journey, and we are here to support you every step of the way. Together, we can work towards a healthier future.
Claudication is a significant sign of Peripheral Artery Disease (PAD), often felt as pain or cramping in the legs, especially during activities like walking. This discomfort occurs when blood flow to the muscles is reduced due to narrowed arteries, primarily caused by atherosclerosis. Many patients describe a heaviness or fatigue in their legs, which usually eases with rest. Recognizing claudication is crucial for the early diagnosis of PAD vs PVD symptoms, as neglecting these signs can lead to serious complications, including critical limb ischemia.
Have you noticed any discomfort in your legs while walking? Recent studies show that intermittent claudication can greatly impact the quality of life for older adults, leading not just to physical limitations but also emotional challenges. Vascular health experts stress the importance of being aware of claudication, as it serves as a vital indicator of PAD vs PVD symptoms, reduced blood flow, and systemic atherosclerosis. One expert pointed out that "walking pain from PAD is referred to as intermittent claudication, which means 'to limp.'" This highlights the need for individuals to seek medical assessment when they experience such symptoms.
Real-life stories illustrate the importance of early detection. Patients who respond quickly to claudication signs often benefit from timely interventions that can prevent further decline in their vascular health, especially when evaluating PAD vs PVD symptoms. By understanding the implications of claudication, you can take proactive steps toward managing your condition and enhancing your overall well-being. Remember, you’re not alone in this journey; seeking help is a strong and positive step forward.

Peripheral Vascular Disease (PVD) can bring about a variety of signs, such as leg pain and swelling, which are included in the pad vs pvd symptoms and may significantly impact daily life. Many patients experience discomfort in their legs, particularly after sitting or standing for long periods, which can be classified under pad vs pvd symptoms, specifically known as intermittent claudication. Thankfully, this discomfort often eases with rest, distinguishing it from the more severe symptoms of Peripheral Artery Disease (PAD). Additionally, swelling in the legs can occur due to fluid retention or venous insufficiency, which are both commonly associated with pad vs pvd symptoms.
Did you know that nearly 10% of the U.S. population is affected by PVD? This number is even higher among older adults. For example, applying the 27.7% prevalence rate to the 2020 population aged 65 and older suggests that around 15.2 million older adults are living with PVD. This statistic underscores the importance of recognizing signs early, as untreated PVD can lead to serious complications, including tissue death and limb loss.
Healthcare professionals emphasize the need for awareness regarding pad vs pvd symptoms. As one expert wisely pointed out, "Without treatment, PVD can progress and cause severe loss of blood flow." This statement highlights the critical nature of prompt diagnosis and tailored management strategies that cater to individual needs.
Managing PVD often involves making lifestyle changes that can greatly improve comfort and quality of life. Regular exercise, maintaining a healthy weight, and wearing compression garments can all help alleviate discomfort. It's also vital to understand the differences between PVD and PAD, as each condition requires specific management approaches. By fostering awareness of pad vs pvd symptoms and their implications, patients can take proactive steps toward better vascular health. Remember, you’re not alone in this journey-support is available, and taking action can lead to a healthier, more fulfilling life.

Peripheral Artery Disease (PAD) can be a concerning diagnosis, and it’s important to understand the factors that contribute to its development. The following factors all play a role:
For older adults, especially those over 65, the risk increases due to the natural aging process and the cumulative effects of lifestyle choices. Recognizing these risk factors empowers individuals to make informed decisions about their health and seek appropriate medical guidance.
At Amavita Heart and Vascular Health, we understand how overwhelming it can be to face health challenges. Our specialists are here to help. We utilize advanced diagnostic imaging to identify blockages caused by PAD, ensuring that you receive the most accurate assessment of your condition. Furthermore, we offer minimally invasive procedures designed to restore blood flow to your legs, significantly improving your walking distance and alleviating pain.
By addressing these risk factors and providing specialized care, we strive to enhance the quality of life for those we serve. Remember, you’re not alone in this journey. Our team is dedicated to supporting you every step of the way. If you have concerns about your health, don’t hesitate to reach out. Together, we can work towards a healthier future.

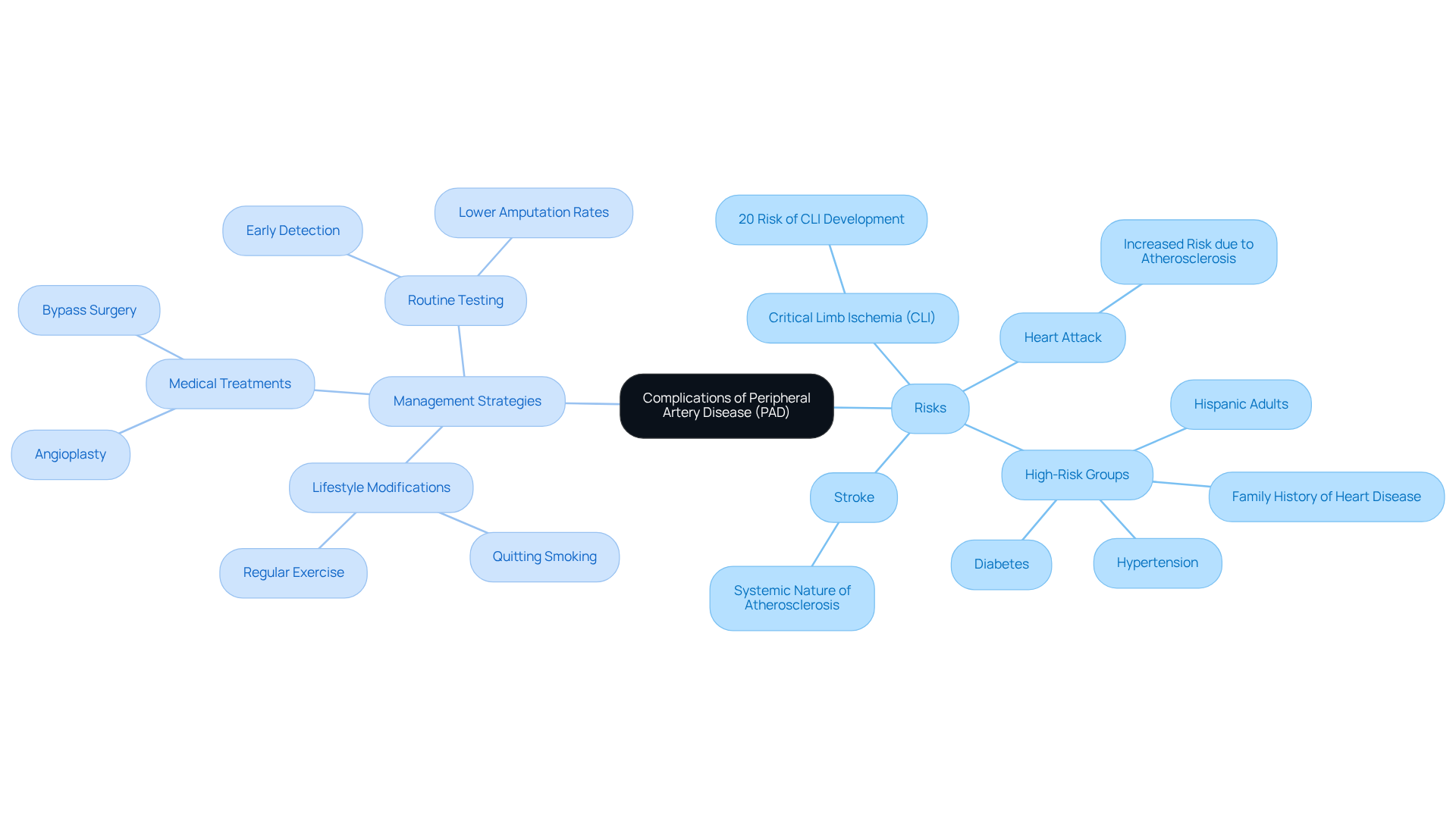
If left untreated, Peripheral Artery Disease (PAD) can lead to serious complications, including critical limb ischemia (CLI), which may result in tissue death and even amputation. This is particularly concerning for individuals with PAD, especially those who have diabetes, hypertension, or a family history of heart disease. These individuals face a heightened risk of heart attack and stroke due to the systemic nature of atherosclerosis.
Did you know that approximately 20% of individuals with PAD may develop CLI? This statistic underscores the importance of early detection and intervention, especially among high-risk groups like Hispanic adults. At Amavita Heart and Vascular Health, we offer advanced imaging capabilities, including ultrasound and angiography, along with comprehensive evaluations. Our goal is to ensure that high-risk individuals receive the targeted cardiovascular care they need.
Understanding these risks is crucial for encouraging individuals to seek therapy and make lifestyle changes that can help reduce these threats. It's essential to consult your healthcare provider for specific medical needs and to engage in proactive healthcare discussions.
Effective management strategies include:
Furthermore, routine testing at Amavita can lead to earlier detection and treatment of PAD, potentially lowering amputation rates.
By understanding these risks and management options, patients can significantly decrease their chances of serious complications. Remember, you are not alone in this journey; we are here to support you every step of the way.
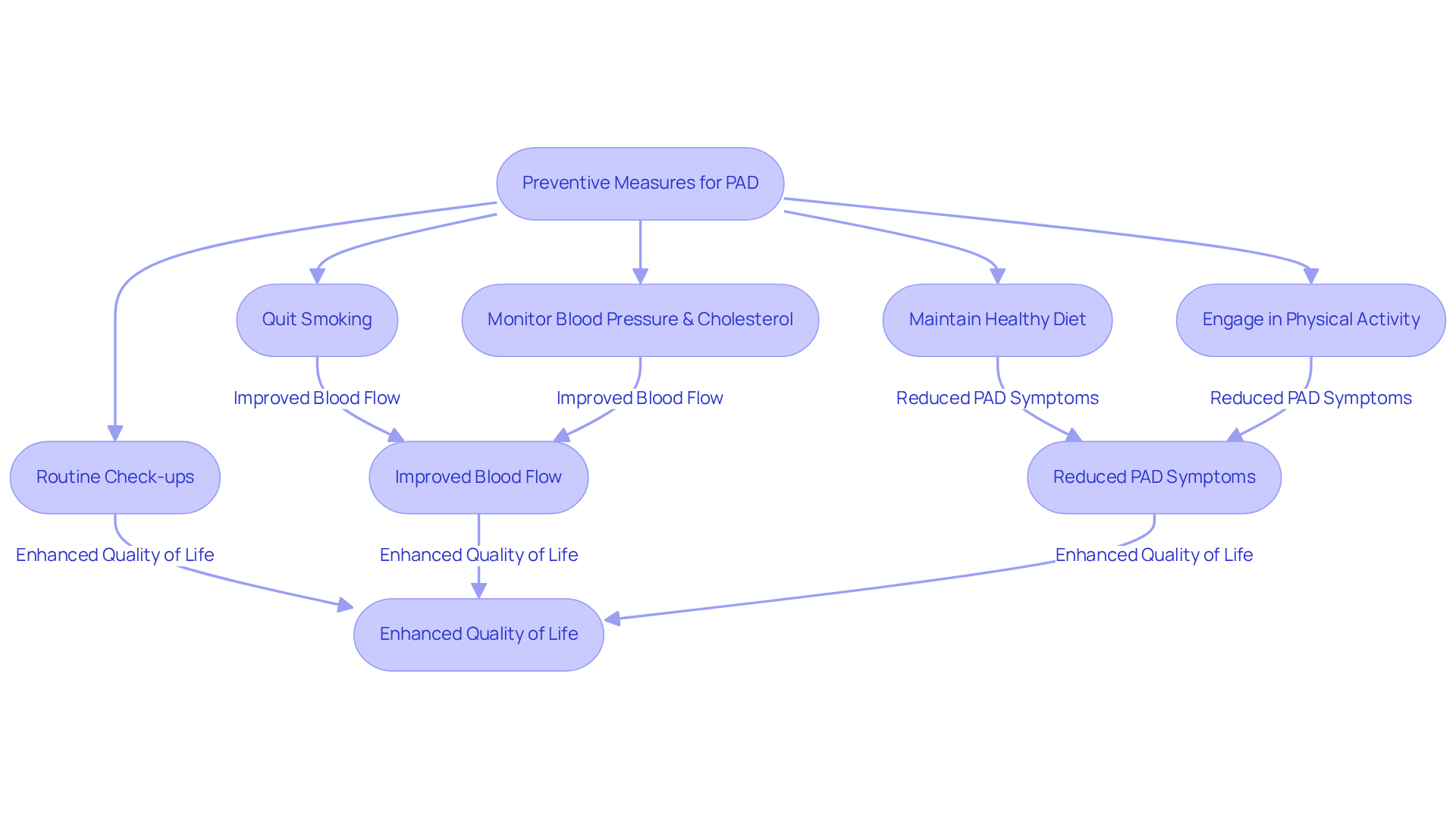
Taking preventive measures for Peripheral Artery Disease (PAD) is essential for managing PAD vs PVD symptoms, which impacts your vascular health and overall quality of life. Have you considered how lifestyle changes can make a difference? One of the most impactful steps you can take is to stop smoking, a significant contributor to PAD. Research shows that individuals who quit smoking often experience improved blood flow and reduced PAD vs PVD symptoms, leading to a more active and fulfilling life.
In addition to this, maintaining a healthy diet is crucial. Focus on incorporating plenty of fruits, vegetables, whole grains, and lean proteins into your meals. This not only helps manage cholesterol levels but also supports your cardiovascular health. Remember, every small change counts!
Engaging in regular physical activity is vital too. Even participating in supervised exercise programs can enhance your walking ability and alleviate pain associated with PAD vs PVD symptoms. It’s important to monitor your blood pressure and cholesterol levels diligently; managing these factors can help prevent the progression of PAD. And if you have diabetes, effective management is equally important, as uncontrolled blood sugar can worsen vascular issues.
Routine check-ups with your healthcare provider can lead to early detection of risk factors, allowing for timely interventions. Current guidelines recommend regular assessments, including the ankle-brachial index (ABI) test, to evaluate blood flow and detect PAD early. By embracing these lifestyle changes and following your medical team’s guidance, you can significantly lower your risk of complications related to PAD vs PVD symptoms, including heart attacks and strokes.
Remember, you’re not alone in this journey. Reach out for support, and take these steps towards a healthier future.
Diagnosing Peripheral Artery Disease (PAD) begins with a thorough physical examination and a careful look at your medical history. One of the most effective tools for diagnosis is the Ankle-Brachial Index (ABI). This test compares blood pressure readings in your ankle to those in your arm. An ABI ratio of less than 0.90 often indicates the presence of PAD, which is crucial to catch early. Did you know that studies show the ABI test is highly reliable? It has proven effective across various demographics, especially for those at higher risk, like individuals with diabetes, hypertension, or a family history of heart disease. In fact, PAD affects up to 25% of adults, highlighting the importance of early diagnosis and management.
In addition to the ABI, Doppler ultrasound is used to assess blood flow and determine the severity of any arterial blockages. This non-invasive technique allows healthcare professionals to visualize blood circulation in real-time, enhancing the diagnostic process. Recent advancements, such as the estimated TBI (eTBI) method, have further improved diagnostic accuracy, particularly for those with diabetes, who are more vulnerable to PAD complications. At Amavita, our advanced imaging capabilities ensure that these sophisticated tests are seamlessly integrated into a personalized care plan tailored to your unique needs.
Vascular specialists emphasize that early diagnosis is essential for effectively managing PAD. As noted by Newman Medical, "The ABI test remains the gold standard for PAD diagnosis in primary care settings." By recognizing the condition promptly, you can start making lifestyle adjustments and treatment choices that significantly reduce the risk of serious complications, including limb loss. For example, lifestyle changes like quitting smoking and improving your diet are vital in managing PAD. Real-life stories show that individuals diagnosed early through the ABI method often enjoy better outcomes and an improved quality of life. Furthermore, supervised exercise programs have been shown to greatly alleviate symptoms and increase walking distance for those with claudication.
Overall, integrating these diagnostic techniques at Amavita is crucial for timely intervention and optimal care. Remember, you’re not alone in this journey; we’re here to support you every step of the way.

When it comes to managing Peripheral Artery Disease (PAD), there are various treatment options available that can truly make a difference. It’s important to understand that lifestyle modifications, medications, and even advanced surgical interventions can all play a role in improving your health and well-being. Simple changes, like quitting smoking, engaging in regular exercise, and following a heart-healthy diet, are essential. These steps not only help manage PAD but can also significantly enhance your overall outcomes.
Medications are often part of the treatment plan, too. Antiplatelet agents, such as aspirin, and statins are commonly prescribed to alleviate discomfort and lower cardiovascular risks. Statins, in particular, are effective at reducing LDL cholesterol and inflammation, which is crucial for those living with PAD.
For individuals facing more severe symptoms, procedures like angioplasty and bypass surgery may be necessary to restore proper blood flow. Angioplasty, often performed with drug-coated balloons, has shown promising success in reopening blocked arteries, thanks to recent advancements that enhance safety and recovery times. Bypass surgery remains a standard option for complex cases, especially when significant blockages are present. Many individuals report significant relief from symptoms and improved mobility after these procedures.
Recent advancements in PAD treatment emphasize a personalized approach, tailoring interventions to meet your unique needs. Innovative methods, such as bioresorbable stents and minimally invasive procedures like the Percutaneous Transmural Arterial Bypass (PTAB), offer new hope for those dealing with severe blockages. These advancements not only improve treatment effectiveness but also shorten recovery times, allowing you to return to your daily activities more quickly.
Ultimately, the choice of treatment for PAD depends on the severity of the disease and your overall health. This highlights the importance of a thorough evaluation by healthcare professionals who genuinely care about your well-being. With over 12 million Americans affected by PAD, understanding these treatment options is vital for improving your quality of life and preventing complications. Remember, you’re not alone in this journey, and there are compassionate resources available to support you.

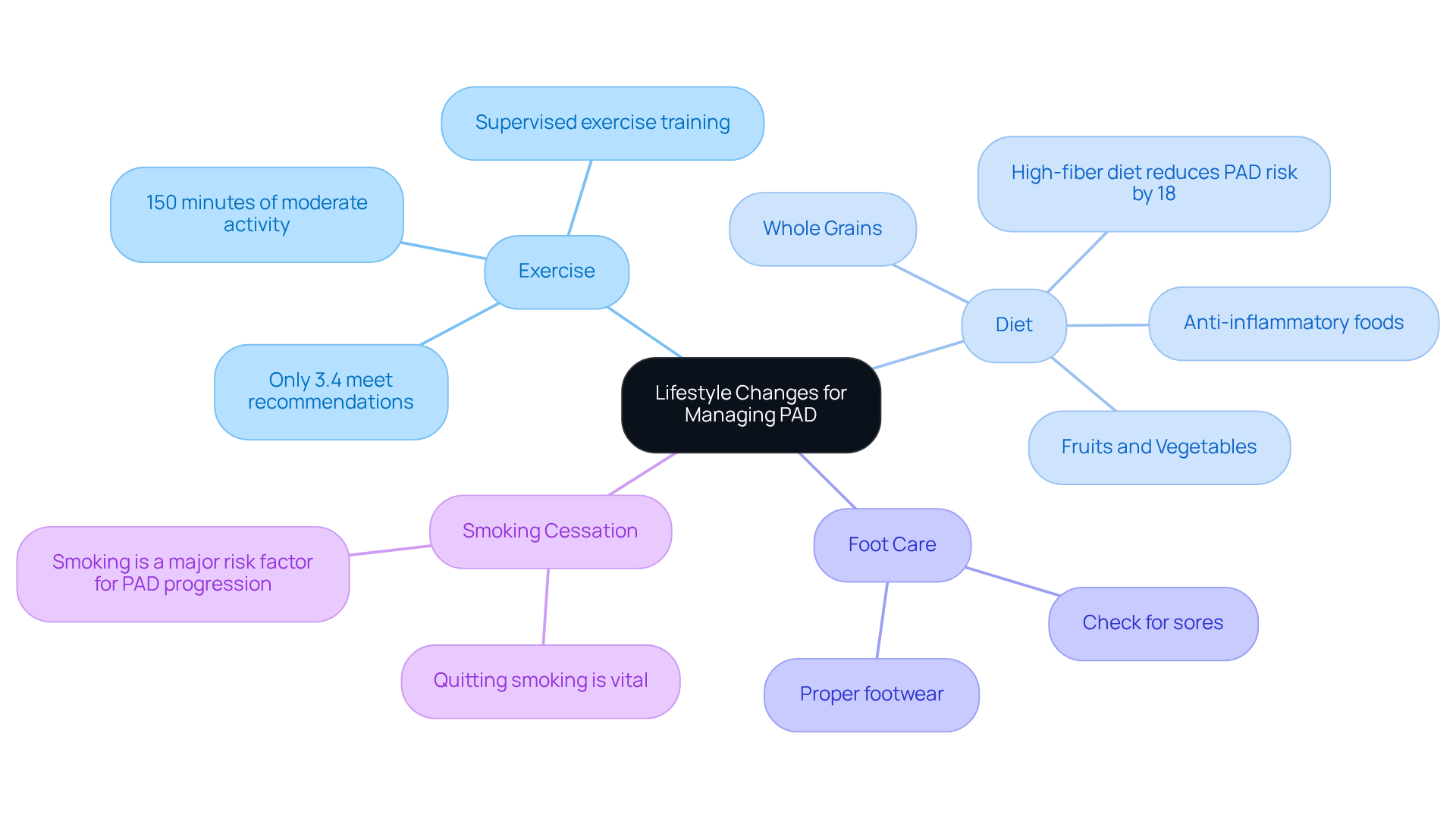
Managing Peripheral Artery Disease (PAD) can feel overwhelming, especially when considering the pad vs pvd symptoms, but making some lifestyle changes can truly make a difference. Have you considered how regular exercise, especially walking, could enhance your circulation and alleviate the pad vs pvd symptoms? Supervised exercise training is a key therapeutic method that not only improves physical function but also boosts the quality of life for those living with PAD. Current guidelines recommend at least 150 minutes of moderate or 75 minutes of vigorous physical activity each week, ideally in sessions of at least 10 minutes. Yet, it’s concerning that only 3.4% of PAD patients meet these recommendations. This highlights the challenges many face in sticking to exercise routines.
In addition to exercise, embracing a heart-healthy diet is essential. Think about incorporating more fruits, vegetables, whole grains, and lean proteins into your meals while steering clear of saturated fats, trans fats, and added sugars. Nutritionists emphasize that these dietary choices can significantly impact cardiovascular health related to PAD. For instance, did you know that a high-fiber diet can lower your chances of developing PAD? Studies suggest that regularly eating fruits and vegetables can reduce this risk by as much as 18%. Furthermore, an anti-inflammatory diet, filled with foods that help reduce inflammation, is also recommended to lower the likelihood of PAD.
Taking care of your feet is another crucial aspect, especially for those with diabetes. Regularly checking your feet for sores or injuries and wearing proper footwear can help prevent complications. And let’s not forget about smoking-quitting is vital for reducing the risk of PAD progression, as smoking is a significant risk factor. By making these lifestyle adjustments-consistent exercise, a heart-friendly diet, attentive foot care, and quitting smoking-you can effectively manage your condition and alleviate pad vs pvd symptoms, thereby improving your overall quality of life. Remember, you’re not alone in this journey; support is available, and every small step counts.
Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) both impact blood circulation, but understanding the unique signs associated with PAD vs PVD symptoms is essential for accurate diagnosis. Are you experiencing leg pain or cramping during physical activity? This could be a sign of PAD, often described as intermittent claudication, which typically eases with rest. On the other hand, PVD may present with persistent swelling, varicose veins, and skin changes like discoloration or ulcers. Misdiagnosis can occur, especially when PAD vs PVD symptoms overlap, which can lead to inadequate treatment and worsening conditions.
Recent studies show that individuals with advanced PAD frequently also deal with chronic venous insufficiency. This highlights the importance of thorough assessments. Experts emphasize that accurate diagnosis is crucial; vascular health specialists note that understanding the differences in PAD vs PVD symptoms can significantly improve outcomes for patients.
For effective management, it’s important to recognize these key differences:
Understanding these distinctions, especially the PAD vs PVD symptoms, not only helps you seek the right care but also prevents the potential consequences of misdiagnosis, such as increased morbidity and mortality associated with untreated PAD. By being aware of these differences, you can have more informed discussions with your healthcare providers, leading to better health outcomes. Remember, you’re not alone in this journey; support is available, and taking the first step towards understanding your health is a powerful move.

Understanding the differences between Peripheral Artery Disease (PAD) and Peripheral Vascular Disease (PVD) is crucial for your health. Both conditions affect blood circulation, but recognizing their distinct symptoms can lead to better outcomes. For instance, PAD often causes claudication, which is pain or cramping in the legs during physical activity. On the other hand, PVD may present as persistent swelling and skin changes. Misunderstanding these symptoms can lead to inadequate treatment, potentially worsening your condition.
In this article, we’ve highlighted key insights, such as the importance of early detection and how lifestyle changes can help manage both PAD and PVD. Factors like age, smoking, and diabetes significantly increase the risk for PAD, while PVD is often linked to prolonged standing and obesity. Understanding the complications of untreated PAD, like critical limb ischemia, emphasizes the urgency of seeking medical attention when symptoms arise.
Ultimately, being aware of the differences between PAD and PVD empowers you to have informed discussions with your healthcare provider. This can lead to timely interventions and an improved quality of life. Taking proactive steps, such as adopting a heart-healthy lifestyle and recognizing early symptoms, is vital for managing your vascular health. Remember, support is available, and by prioritizing your cardiovascular well-being, you can navigate your health journey with confidence.
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease (PAD) is a condition characterized by narrowed arteries that reduce blood flow to the limbs, often leading to symptoms such as pain or cramping in the legs during activities like walking.
What are the symptoms of PAD?
Common symptoms of PAD include claudication, which is pain or cramping in the legs during physical activity, and discomfort that typically eases with rest. Other symptoms may include heaviness or fatigue in the legs.
How does PAD differ from Peripheral Vascular Disease (PVD)?
While PAD specifically refers to narrowed arteries affecting blood flow to the limbs, PVD is a broader term that encompasses various conditions affecting blood vessels, including leg pain and swelling. PAD is a type of PVD.
What is claudication and why is it important?
Claudication is a key symptom of PAD, often described as pain or cramping in the legs during activities. It is important because recognizing claudication can lead to early diagnosis and intervention, preventing more serious complications.
What treatments are available for PAD?
Treatments for PAD include advanced, minimally invasive procedures such as drug-eluting stents and atherectomy devices, which improve blood flow and reduce discomfort. Each treatment plan is personalized to meet the patient's unique needs.
How can lifestyle changes help manage PVD?
Lifestyle changes such as regular exercise, maintaining a healthy weight, and wearing compression garments can alleviate discomfort associated with PVD and improve overall quality of life.
What should I do if I experience symptoms of PAD or PVD?
If you experience symptoms such as leg pain or claudication, it is important to seek medical assessment. Early detection and intervention can significantly improve vascular health and quality of life.
Is there support available for individuals with PAD or PVD?
Yes, support is available for individuals dealing with PAD or PVD. Healthcare providers, community outreach initiatives, and innovative research efforts are in place to assist patients in managing their conditions effectively.